-
Enhancing Patient Outcomes in Obstetrics Care: The Role of Quality Improvement
In recent years, maternal health in the United States has been declining. According to the Centers for Disease Control and Prevention, the maternal death rate in the US has risen steadily over the past decade, with the majority of these deaths being preventable. Combating this trend through quality improvement in obstetrics care has become a central focus. By implementing standardized care based on best practices and providing effective training, healthcare organizations have the power to significantly improve outcomes in obstetrics care and ensure patient safety.
The Impact of Quality Improvement
Quality improvement initiatives play a crucial role in achieving better patient outcomes in obstetrics care. Initiatives such as perinatal reviews and maternal quality collaboratives bring together healthcare providers from across the system to discuss and learn from cases of adverse outcomes, leading to performance improvement. Most healthcare organizations acquire international certifications, like the Joint Commission International Accreditation (JCIA), and accreditation of hospitals that recognize excellence in perinatal medicine. These initiatives ensure adherence to prescribed protocols and guidelines.
An example of standard care protocol success is a study on the California Maternal Quality Care Collaborative (CMQCC) Toolkit that provides approaches and strategies for providing care to women with maternal hemorrhage, hypertension, and severe sepsis. The implementation of this Toolkit averted 913 cases of severe maternal morbidity (SMM), 28 emergency hysterectomies, and one maternal death. It also resulted in $9 million saved.
The success of the Toolkit lies in its standardized, evidence-based protocols that greatly improve clinical management. “Quality improvement efforts in maternity care not only save lives; they can save costs,” said study co-author Elliott Main, MD, clinical professor of obstetrics and gynecology at Stanford Medicine and medical director of the California Maternal Quality Care Collaborative. Dollars saved can be reinvested into staff training to further improve maternal care and outcomes. For so many health systems that follow Joint Commission standards but still fall short of their patient safety goals, effective training is the link between having standards in place and ensuring standardized action and care. But implementing successful quality improvement training at scale can be challenging. Here are some critical points to consider.
Steps to successful quality improvement in obstetrics care
1. Utilizing the power of data analytics and technology
Obstetrics care also benefits significantly from data analytics and technology as the application of business intelligence systems can help monitor and analyze large volumes of data to identify likely adverse events. Predictive analytics can help detect early warning signs and intervene before an adverse event occurs. The use of electronic health records makes data recording, graphing, and analyzing easy, which can help identify deviations from standard care practices with ease. Technology also empowers patients to participate in their care plan by accessing data at any time and communicating with healthcare providers.
2. Reinforcing established standard practices with effective training
Establishing standard care processes, such as the Joint Commission’s, is just the beginning. It is equally important to ensure that these practices are understood, followed, and regularly updated. But simply offering training is not enough — clinicians need fast and effective training that works. Otherwise, the standard best practices health systems work so hard to identify and develop are useless. Continuous improvement of skills and knowledge, rigorous training exercises, and assessment can significantly enhance performance. By delivering safe and effective treatment during pregnancy, childbirth, and the postpartum period, healthcare providers can make a tangible difference in patient outcomes.
3. Prioritizing patient equity
Centers for Disease Control and Prevention (CDC) data reveals that American Indian/Alaska Native and Black women are 2 to 3 times as likely to die from a pregnancy-related cause than white women, among other figures that indicate racial disparities in obstetrics care and patient outcomes. Although this data created much-needed awareness around this issue, simply recognizing the problem does not translate to improved outcomes. Quality and improvement teams need clear action plans around this issue to be reinforced with effective training. Obstetrics departments that successfully tackle this gap in care will set themselves apart from those who do not make it a priority.
4. Emphasizing patient empowerment and informed consent
Patient empowerment is critical to enhancing obstetrics care outcomes and maximizing quality improvement efforts. Research indicates that patient education efforts have been proven to lead to more positive outcomes. Care goes beyond applying procedures or making a diagnosis. Patients and their families need to embody trust and collaborate in partnership with healthcare providers, enabling better decision making, and developing the understanding that supports shared goals and transparent communication. This way, patients are better empowered to make informed decisions about their care.
The declining maternal health statistics in the United States are alarming, and it is up to us as healthcare providers to adopt data-driven standardized care, reinforced by effective training, to enhance patient outcomes in obstetrics care. Implementing standard care practices, revisiting continuous learning and training, utilizing data analytics and technology, and empowering patients are just some of the critical elements that can be expanded upon to set the system on a positive trajectory. It is vital that those decision-makers who oversee care delivery invest in these strategies and make addressing the decline in maternal health statistics a priority. Ultimately, this will improve obstetrics care, increase maternal and infant safety, and empower women in their healthcare.
-
New Analyst Report Profiles Amplifire’s Remarkable Learning Outcomes and Unique AI Capabilities
Analyst firm Brandon Hall Group recently profiled Amplifire, digging into healthcare outcomes like measurable increase in proficiency, 79% reduction in CLABSI incidence, and millions of dollars in cost savings as well as its unique use of AI to transform course content development. At a time when health systems are facing steep challenges that require innovative, efficient, and effective solutions, technology that improves margins, boosts clinician satisfaction, and enhances patient safety makes all the difference.
Read their Solution Provider Profile to learn how Amplifire:
- Expedites learning by cutting training time
- Boosts retention through embedded, cutting-edge cognitive science discoveries
- Measurably improves performance following training
- Offers industry-disrupting content authoring capabilities with AI and best-in-class, peer development opportunities
-
4 Key Takeaways from the recent Becker’s Healthcare Webinar: How Innovative EHR Training Can Improve Clinician Well-Being
As we are all aware, healthcare is experiencing widespread burnout, with a staggering 77% of healthcare providers reporting varying degrees of stress or burnout. Through extensive research, the KLAS Arch Collaborative, a group of healthcare organizations committed to improving the EHR experience through shared research, standardized surveys, and benchmarking, has identified EHR-related factors as burnout contributors. But the good news is, pinpointing specific EHR experience factors, like tool inefficiency, lack of training, poor proficiency, allows for directed intervention and improvement.
Recently, during the Becker’s Healthcare webinar titled “How Innovative EHR Training can Enhance Clinician Well-being,” experts delved into the realm of EHR training, sharing insights on successful strategies and pitfalls to avoid. Jenna Anderson, representing the KLAS Arch Collaborative, presented illuminating data on optimizing the EHR experience through personalized training and enhanced user engagement. Erin Banaszak provided a compelling glimpse into Froedtert Health’s successful journey in EHR training transformation.
For healthcare systems looking to reinvent their approach to EHR training with the goal of elevating clinician satisfaction, well-being, and overall organizational effectiveness, this article offers four essential takeaways from the enlightening webinar.
1. The experience with initial EHR education is critical to clinicians’ overall satisfaction.
First impressions are everything — even (and especially) when it comes to EHR training and onboarding. Data suggests that use of a certain EHR vendor doesn’t guarantee user satisfaction. So, if it’s not the vendor creating this varying experience, what is it?
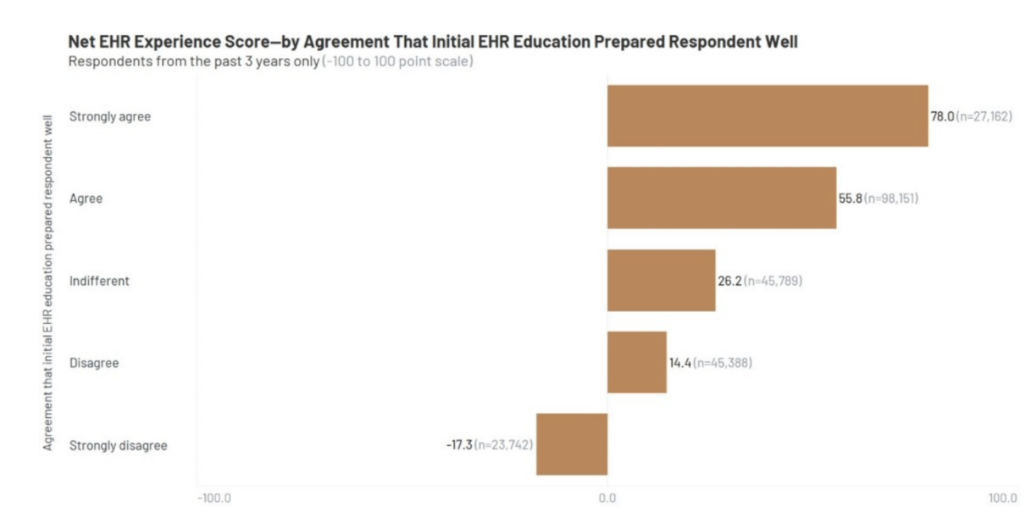
KLAS dove deeper into the connection between EHR experience and EHR education. Using a Likert scale, KLAS measured how well initial EHR education prepared clinicians to use the EHR. Correlating those responses with a user’s Net EHR Experience Score (ranging from -100 to +100), users who strongly agree that their initial training prepared them well score 78.0, whereas users who strongly disagree that their initial training prepared them well score a -17.3. This revealed a 95-point difference in user satisfaction — just based on initial training! That difference reveals a major opportunity for improvement.
2. Clinicians want more training! But there’s a catch.
To the survey question asking respondents if they want more EHR training, over half said they do! As surprising as it is to see that result, it comes with a big catch. It’s likely that of the clinicians who responded “yes” to more training, they aren’t imagining signing up for more timein a classroom.
In other words, more training doesn’t mean longer training. More training means more high-quality training. As a follow-up to this survey, Jenna Anderson, strategy and operations director from KLAS Arch Collaborative, shared provider feedback about what kind of training they wanted more of. Responses included: “better training up front and subsequently,” “more videos,” “improved specialty-focused training,” and “better access to training materials.”
If an organization’s training is not meeting clinicians where they are, it doesn’t mean training doesn’t work. It means training needs to be better, because clinicians want effective, efficient training. This also applies to the 46% of respondents who replied that they didn’t want more training, assuming the training experience was lacking to them in some way.
3. Online learning that prioritizes science-based retention methods is the biggest differentiator in terms of time savings.
Data indicates that self-directed eLearning has the biggest impact on time savings (above other forms like virtual instructor-led training or classroom training), but when powered by brain science-based methodology, it boosts results.
KLAS data indicates that 91 EHR minutes are saved per week for every one hour of training with self-directed eLearning, whereas the next closest category, in-person one-on-one training saves just 72 minutes. EHR minutes saved are minutes given back to the clinician to focus on what they want to do most: provide high-quality care.

image: https://klasresearch.com/archcollaborative/report/clinician-training-2023/480
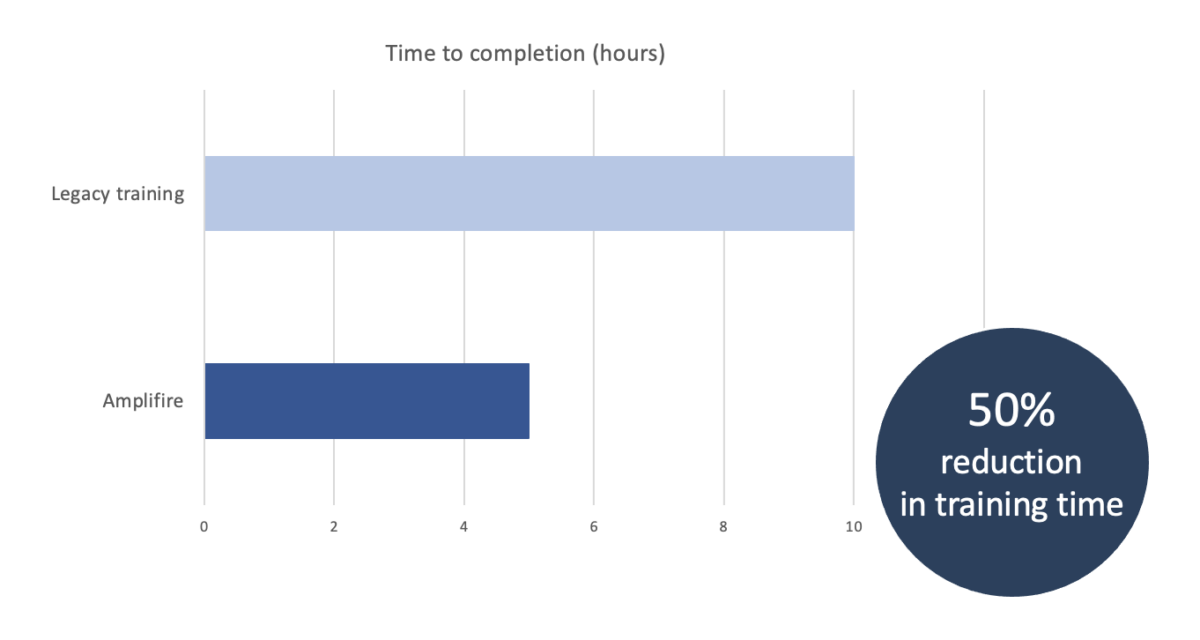
When this self-directed eLearning takes the form adaptive, personalized learning powered by brain science-based learning methodology, it cuts training time even more, targets knowledge gaps, and ensures proficiency, translating to even less time spent in the EHR. For FroedtertHealth, who used self-paced online learning via LMS, switching to adaptive online learning shaved an additional 50% from training time, getting clinicians back on the floor faster, helpingmore patients, and logging more billable hours. This also ties right back to the fact that clinicians want more training. If training is personalized and adapts to each learner’s needs, they learn only what they don’t already know, maximizing training efficacy and boosting the clinician experience by not wasting their time.
4. Robust data and learner insights impact clinician satisfaction and well-being.
Robust learner analytics are the key to doubling down on learning personalization and training optimization. When organizations have access to hidden insights, such as pinpointed knowledge gaps, learner struggle, and confidently held misinformation, they can create individualized remediation plans for specific learners — getting them the coaching they need, sooner.
But deep insights like this help health systems optimize their training program at large. Learner insights reveal what prior knowledge their learners have, allowing them potentially place learners on different tracks. For example, Froedtert Health’s learner data pinpointed consistently low levels of struggle among certain clinicians, so those clinicians are placed on an accelerated plan, thus saving time while respecting learners’ expertise. For clinicians that demonstrated high struggle levels, they are placed on a supportive track to ensure they get the learning they need to be highly proficient. This is different than simply asking if clinicians have prior experience with a particular EHR vendor — some clinicians that indicate that they do have prior experience still demonstrate high levels of struggle. In that case, they will get the support they need (that they may not have otherwise gotten without the deep learner data). From identifying incoming clinician learning trends, they refine their training program to ensure efficiency and efficacy to boost clinician satisfaction. With a training program that is rigorously personalized to clinicians’ needs, their well-being improves. They get the training they want and the learning they need, right when they need it.
This webinar shed light on effective strategies to improve the EHR experience and, by extension, clinician satisfaction. With key takeaways, including the critical role of initial EHR education, the need for more efficient and personalized training, the time-saving potential of self-directed eLearning, and the power of robust learner insights, healthcare systems have the tools to revolutionize their approach. To delve deeper into these insights and elevate clinician satisfaction and organizational effectiveness, watch the full webinar.
-
Why Effective Obstetrics Training Matters More Than Ever
Despite continuous medical advancement, the risk of maternal mortality and morbidity is increasing. The Center for Disease Control and Prevention data shows that the US maternal death rate rose sharply in 2021. This alarming figure follows in the wake of a global pandemic, where caution and safety were at the forefront of clinicians’ minds. Moreover, while maternal mortality rates have decreased 43 percent, globally, since 1990, the US is the only developed country where it has increased. The problem only becomes graver from a demographic perspective, where American Indian/Alaska Native and Black women are 2 to 3 times as likely to die from a pregnancy-related cause than white women.
Why is the US trailing behind other developed countries when it comes to maternal health? In a time where clinician burnout is rising and organizations face high turnover rates, the US not only saw maternal health decline, but patient safety as a whole. A 2022 literature review by senior leaders in health systems directly dealing with patient safety issues, stated that “Patient safety policy and practice has relied too heavily on the vigilance and heroism of clinicians, rather than the design of safe systems.” And in response to recent patient safety declines, they propose proven-effective training combined with standardized care processes to improve outcomes.
Now, more than ever, health systems need obstetrics training they can trust; meaning, training that works. In the new age of online learning, it can be difficult to distinguish between what works and what doesn’t, and what meets high-performing health systems’ standards, and what falls short. Here’s what to look for in an online learning platform for obstetrics training.
-
Boost Clinician Satisfaction & Maximize EHR ROI by Enhancing the Learning Experience with Online Learning
In today’s rapidly evolving healthcare landscape, the challenges facing health systems are more complex than ever. High burnout rates, clinician turnover, and low satisfaction among healthcare professionals have become pressing issues that demand immediate attention.
Unhappy and overburdened clinicians are more prone to making errors, leading to compromised patient safety and outcomes. Dangerous clinician burnout is only exacerbated by documentation burdens. Herein lies the importance of proper EHR training. Efficient use of EHRs can significantly improve clinical workflows, allowing healthcare professionals to focus more on patient care and less on administrative tasks. They get back to doing what they love, with less friction. In turn, clinician satisfaction improves, and health systems experience less turnover.
Implementing online learning in a blended learning environment to improve the EHR learning experience
In the quest to improve EHR training experiences and, subsequently, clinician satisfaction, health systems are getting innovative. An approach that allows for creativity is blended learning.
In its simplest form, blended learning is education consisting of two or more delivery methods. By combining different delivery methods, blended learning offers a more dynamic and interactive learning environment. For example, health systems use Amplifire’s online learning platform as part of their overall learning ecosystem.
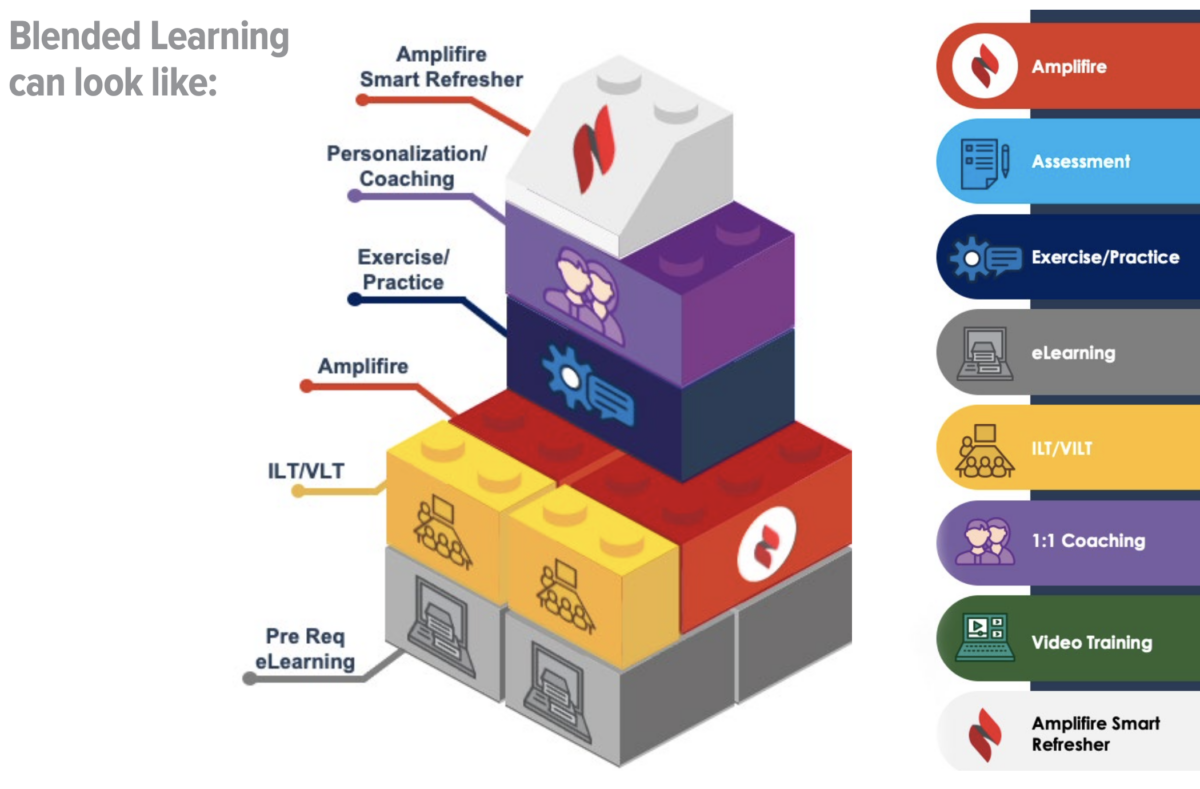
Organizations that have incorporated adaptive online learning into innovative blended learning ecosystems have seen measurable improvement in training time, EHR proficiency, and clinician satisfaction. To explore these results, blended learning best practices, and provide actionable steps to implement adaptive EHR training programs effectively, download the free eBook.
-
Recognizing Sepsis Awareness Month: Online learning for better patient outcomes
Regrettably, at least 1.7 million adults in America develop sepsis each year, leading to at least 350,000 sepsis-related deaths in the United States. On average, 87% of sepsis cases originate outside the hospital.
As sepsis continues to be a pressing issue in healthcare, action must be taken. Recently, in her first major initiative rollout as the director of the CDC, Dr. Mandy Cohen released the CDC’s Hospital Sepsis Program Core Elements. These guidelines offer a detailed roadmap for hospitals to follow to reduce deaths from sepsis in their facilities.
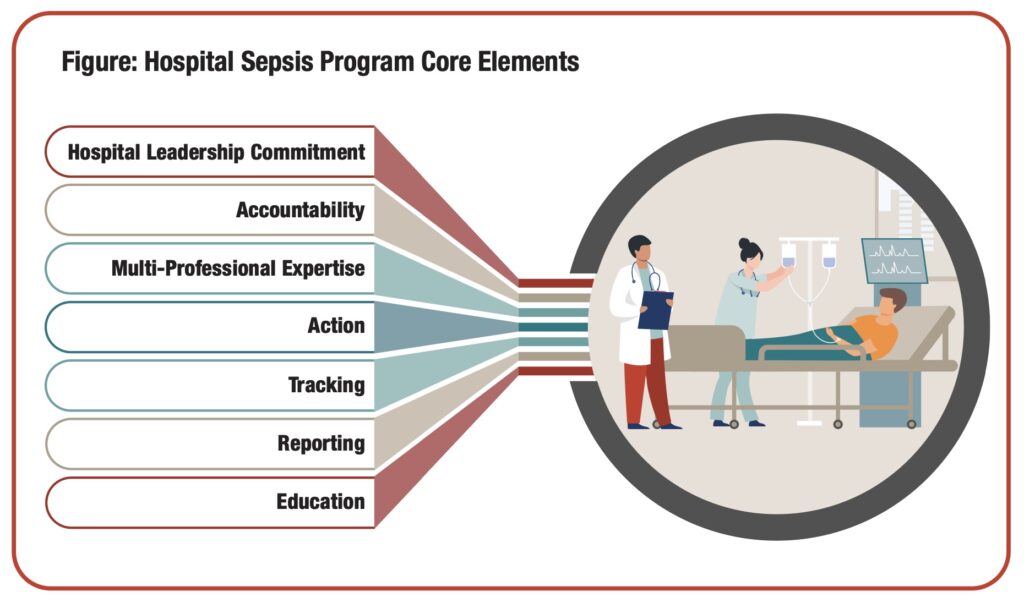
One of the seven core elements outlined in this roadmap is education. The CDC recommends, “For optimal sepsis treatment and outcomes, it is imperative that hospital staff have strong knowledge of sepsis and understand their role in team-based management of sepsis.” Examples of priority sepsis education include:
- Including sepsis-specific training and education in the hiring or on-boarding process for healthcare staff and trainees
- Providing annual sepsis education to clinical staff
The implementation of unified standard best practices delivered via effective education has been shown to improve patient safety, and can be applied to sepsis treatment, too.
A 2022 systemic review of thirty-two studies on the impact of sepsis education for healthcare professionals on patient outcomes concluded that most educational programs had an effective and immediate impact on knowledge levels, and simulation and game-based programs yielded better outcomes overall. It also concluded that, “Improvements in patient care processes and patient outcomes were associated with the concomitant existence or implementation of a hospital sepsis care bundle.” Effective training matters when standard best practices information needs to stick.
For example, central line-associated blood stream infections (CLABSIs) are often preventable — like sepsis — and rates can be reduced, if not eliminated, by adherence to evidence-based patient safety guidelines, reinforced by effective training. One hospital in a large Colorado healthcare system was selected to pilot the idea that CLABSIs could be addressed with training. After implementing Amplifire’s online learning platform, they experienced a 79% reduction in CLABSIs. A reduction of this magnitude has a profound effect, starting with improved patient outcomes, more confident and competent clinicians, a better bottom line, and most importantly, lives saved.
Want to learn more about how effective online learning can lead to decreased sepsis incidents and improved patient outcomes? Reach out. For more information about available sepsis courses, browse our course catalog.
-
Reducing Systems-Level Clinician Burnout Through Data-Driven EHR Training
Clinician burnout is a critical issue that affects the well-being of healthcare professionals and compromises patient care. While electronic health record (EHR) systems are intended to streamline processes and maximize efficiencies, they have inadvertently contributed to clinician burnout by introducing complex workflows and documentation burden.
A 2022 survey by the Harris Poll for athenahealth reveals the complicated relationship between clinicians and EHR systems. On one hand, the physicians surveyed overwhelmingly endorse technology with 90% saying better patient data would instill more confidence in their ability to support patient needs. Moreover, 85% say the patient experience is better with easier access to data. 78% say they have sufficient information about medical history and the context for patient visits, and 71% report EHR platforms allow them to provide high-quality care.
On the other hand, 59% of physician respondents say they are frustrated by the challenges of accessing clinical information on a weekly basis, and 58% say they often (once a week or more) feel stress because of information overload. Also, according to the survey, the leading cause of regular burnout is excessive documentation requirements (57%). Additionally, 91% of respondents say the burden of regulatory requirements is getting worse, 72% do not believe their organization is working to reduce the time they spend on administrative tasks so they can focus on patient care, and 63% express feeling overwhelmed by administrative requirements and burdens on a weekly basis.
So, while clinicians do see the value in EHR systems, they are perpetually frustrated by inefficient processes and documentation/administrative requirements. As those in healthcare know, no two EHR systems are alike. For instance: a clinician may have years of EHR experience but they need to understand a new organization’s or department’s workflow — customizations, nuances, and all. An adaptive online learning platform offers a two-pronged solution to improving systems level burnout: reduces time spent training and simultaneously collects data to optimize EHR processes.
Reduce training time and streamline care with adaptive online learning
Hospitals onboarding clinicians — new or experienced and anywhere in between — can streamline the EHR training process with the help of adaptive online learning. Traditional training methods often involve lengthy in-person sessions, which can be time-consuming and disruptive to clinicians’ workflows. With an adaptive online learning platform, healthcare organizations can provide a personalized learning experience that caters to individual learning needs. Adaptive learning ensures new clinicians get all the information they need, while experienced trainees don’t spend time learning what they already know. Incorperating adaptive online learning into any blended training program greatly reduces time spent learning, reduces costs, and gets clinicians on the floor treating patients faster.
By tailoring the training experience, clinicians can efficiently acquire the necessary skills to better navigate EHR systems, reducing frustration and minimizing the impact on their workload. A study by the KLAS Arch Collaborative, “the single greatest predictor of user experience is not which EHR a provider uses nor what percent of an organization’s operating budget is spent on information technology, but how users rate the quality of the EHR-specific training they received.” Across organizations included in the study, there were 475 instances in which two physicians of the same specialty using the same EHR system in the same organization reported opposing responses as to whether EHR enables them to deliver high-quality healthcare (the response choices were “strongly agreed” or “strongly disagreed”). In over 89% of these instances, the physician who strongly agreed also reported better training, more training efforts, or more effort expended in setting up EHR personalization. Higher quality training equates to more efficient work and higher clinician satisfaction.
Furthermore, doctors with high EHR satisfaction are nearly five times more likely to report they’ll stay at their organization. In a time of labor shortages and widespread burnout, organizations cannot afford to overlook how their EHR training delivers in terms of efficacy and quality of learning experience.
How your online learning platform can help optimize your EHR system
In addition to reducing training time and improving the EHR experience, an online learning platform can contribute to the optimization of EHR processes. These platforms collect valuable data on learner interactions, system usage patterns, and user feedback. By leveraging this data, healthcare leaders can gain insights into the specific challenges clinicians face when using the EHR system to make informed system-level improvements. This information can be used to identify areas for revision, streamline workflows, and enhance usability. With the guidance of informatics leaders, hospitals can collaborate to implement necessary changes and updates based on the collected data, ultimately resulting in a more user-friendly and efficient EHR system.
Additionally, learner data can be used to identify skilled and highly proficient EHR users for future training. It can also identify struggling users and narrow down which topics they have the most trouble with, enabling informed one-on-one coaching, small group lab training, and other interventions.
Reducing systems-level clinician burnout through data-driven EHR training requires the collaboration and support of key decision makers. By leveraging adaptive online learning platforms, healthcare organizations can reduce training time while simultaneously collecting valuable data to optimize EHR processes. Through effective leadership and collaboration, hospitals can foster a culture of continuous improvement, ultimately leading to improved clinician well-being and enhanced patient care.
From the beginning, Amplifire has relied on innovative brain science to guide its product development to create the most effective learning and training solution, perfectly tailored to the way the human brain works. Learn more about how Amplifire helps people learn better and faster with online learning by requesting a demo.
-
3 Strategies for Improving Workplace Safety for Healthcare Staff
As a healthcare professional, you wouldn’t expect to go to work and encounter violence. You show up to take care of patients and promote wellness. But, as if mounting pressures from staff shortages and work overload haven’t taken enough of a toll on staff, workplace violence rates in healthcare settings are climbing.
In the second quarter of 2022, two nurses were assaulted every hour, on average. That translates to 57 assaults per day and 5,200 assaults total. In the first few months of 2022, nearly half of nurses reported a small or significant increase in workplace violence, marking a 57-percent increase from survey findings in September 2021, and a 119-percent increase from March 2021.
With figures like these, healthcare workers are concerned for their safety when they go to work. Patient care becomes more complicated at a time when it desperately needs relief. Furthermore, exposure to aggressive patients negatively impacts medical teams’ diagnoses and procedural performance, resulting in increased likelihood of medical error.
As stressors in the healthcare space have been exacerbated by the pandemic, it’s difficult to pinpoint who or what is at fault for the rise in violent incidents towards healthcare staff. However, what we do know is that both staff and patients are less safe when numbers are on the rise. So, what can we do? How do we actually decrease violent incidents and increase workplace safety to protect healthcare staff?
Workplace Safety Legislation
One crucial step towards protecting healthcare staff from workplace violence is the implementation of workplace safety legislation. The medical community is urging the government and regulatory bodies to recognize the urgency of the situation.
As part of its legislative priorities, the American Nurses Association has called on Congress to pass the Workplace Violence Prevention for Health Care and Social Service Workers Act. This act would require the Occupational Safety and Health Administration to develop and enforce industry-specific workplace safety standards for healthcare employers.
The American Hospital Association and other provider groups are also working to criminalize assault or intimidation of hospital workers by urging Congress to enact the Safety from Violence for Healthcare Employee Act.
Recently, the Occupational Safety and Health Administration (OSHA) began developing a new standard called “Prevention of Workplace Violence in Healthcare and Social Assistance.” In March 2023, OSHA took the first step by convening a Small Business Advocacy Review (SBAR) panel. This panel provides representatives from small businesses and small local government entities with the opportunity to contribute their input during development phases. Rulemaking will be focused on Type-II workplace violence situations, which involve violence perpetrated by patients, clients, and visitors in healthcare facilities.
Initiatives like these are where healthcare leadership is working to move the needle on workplace safety. However, there are things health organizations can be doing on the ground to decrease workplace violence in a tangible way in the meantime.
Workplace Violence Prevention Strategies
In addition to legislation, healthcare organizations must prioritize enacting effective workplace violence prevention strategies. Here are three strategies to consider:
Encourage safe dressing
Implement clear identification protocols for staff, such as badges or uniforms, to ensure that patients can easily identify authorized personnel. This reduces the risk of mistaken identity and potential violent encounters.
Additionally, National Institute for Occupational Safety and Health (NIOSH) recommends:
- Removing anything that could be used as a weapon or taken
- Hair should be tied back so it cannot easily be pulled
- Avoiding wearing loose hanging earrings or necklaces
- Avoiding overly loose clothing could get caught on something and overly tight clothing can restrict movement
- Use breakaway safety cords or lanyards for name tags, keys, etc.
Use violence risk assessment tools
Leverage technology and employ violence risk assessment tools that consider factors such as patient history, past incidents, and behavioral indicators to identify individuals at a higher risk of displaying violent behavior. Early detection allows for appropriate precautions to be taken.
Three recommended tools include: Triage Tool, Indicator for Violent Behavior, and Danger Assessment Tool.
Provide comprehensive training
Prepare your healthcare staff with comprehensive training on de-escalation techniques, conflict resolution, and self-defense. These skills empower employees to effectively manage potentially violent situations and protect themselves and their colleagues.
Training has been shown to effectively decrease workplace violence rates. For example, UCHealth enrolled their staff in an online course covering standard processes to prevent or de-escalate workplace violence. After training, violent incidents decreased by 34%, reported 11% decrease in violent restraint utilization, and employee de-escalation confidence metrics increased by 5%, indicating staff felt safer following training, even if an incident hadn’t occurred.
As workplace violence rates continue to rise in healthcare settings, staff need action on behalf of their organizations. Passing workplace safety legislation, including regulation enforcement, perpetrator criminalization, and standard process development lays the foundation for a safer environment. Concurrently, healthcare organizations should continue to refine strategies like safe dressing, violence risk assessment tools, and comprehensive training to mitigate violence risks. By prioritizing staff safety, we can protect healthcare professionals, improve patient care, and foster a violence-free healthcare environment. Collaboration among healthcare leaders, policymakers, and stakeholders is essential in addressing this urgent issue and ensuring the well-being of both staff and patients.
From the beginning, Amplifire has relied on innovative brain science to guide its product development to create the most effective learning and training solution, perfectly tailored to the way the human brain works. Learn more about how Amplifire helps people learn better and faster with online learning by requesting a demo.
-
Addressing the Nursing Shortage By Reimagining Support Role Training with Online Learning
The Nursing Shortage and Filling the Gaps
As much as hospitals and health systems may fear the implications of the word “burnout,” their peers are right along with them — no one is immune to the devastating ripple effects of the pandemic. And the widespread result of healthcare worker burnout — among other factors such as increased demand for healthcare services — has created a staff shortage, particularly at the nursing level. This shortage has been exacerbated by the lack of incoming nurses (the United States would need to more than double the number of new graduates entering and staying in the workforce for the next three years straight to accommodate the existing gap). Feeling the pressure of a nursing gap this large, over 300 hospital CEOs ranked personnel shortages as their number-one concern in 2021, with 94 percent ranking the registered nurses deficit as the most pressing category.
Most importantly, this shortage is leaving a major gap in patient care and the situation is becoming increasingly urgent. Will this be the catalyst health systems need to get innovative and reimagine clinical education and develop new care delivery models to reduce workload burden?
Benefits of online learning for workforce development
Modern problems require modern solutions, and hospitals are discovering that online learning can be a faster and more effective way to develop more nursing support roles as solution to address the staffing shortage. Prioritizing nursing support roles enables health systems to develop candidates with little to no healthcare experience, but who are interested in the field. With online learning, hospitals can train candidates efficiently, getting care providers on the floor faster and better prepared to provide top-notch patient care. For example, UCHealth took a creative approach with their care model innovations and developed courseware to rapidly grow their Patient Care Assistant program, supporting their nursing personnel and diversifying their workforce.
Hospitals across the country embrace online learning as part of a blended learning program to make training accessible to more candidates but maintain a positive and effective learning experience. This approach allows for more personalized pathways, making it easier for learners to balance work and education. Here are the benefits to using online learning for both health systems and learners to train nursing support staff:
Flexible for learners with different backgrounds
Health systems are finding that care models that disproportionately rely on registered nurses (RNs) are no longer sustainable. Online learning offers flexibility that allows them to meet the diverse needs of candidates who are interested in the healthcare space but may not have experience, English isn’t their first language, are balancing responsibilities, or who struggled in traditional learning settings.
The learning experience is personalized
Online learning with adaptive functionality creates a more personalized learning experience than traditional learning. Adaptive learning platforms can modify the content and pace of learning to the individual learner’s needs and skill level. This can help to ensure that the learning is more effective and engaging — this often results in higher learner satisfaction levels, too.
Faster than traditional learning
When learning is tailored to individuals and their own knowledge levels, online learning via an adaptive platform is faster than traditional learning because it only focuses on what they need to know. Hospitals can train nursing support staff efficiently, getting them on the floor faster — which is crucial in addressing staffing shortages.
Learner data enriches in-person instruction and clinical practice sessions
Additionally, in-person instruction and clinical practice sessions can be enriched by the learner data captured by the online learning system. This data identifies areas of strength and weakness, allowing for more targeted training. Insights collected during online learning are useful for instructors leading hands-on training and clinical sessions.
The pressures of the nursing shortage will not be easing up any time soon. However, online learning has emerged as a practical solution to address the staffing gap by providing personalized, efficient, and flexible training for nursing support staff. The benefits of online learning not only help develop the workforce that enables new care delivery models, but also have the potential to improve the quality of patient care by leveraging learner data to enrich in-person instruction and clinical practice sessions. As healthcare continues to evolve, innovative care models and blended training supported by online learning will play a crucial role in meeting the workforce development needs of the industry and ensuring excellent patient care.
From the beginning, Amplifire has relied on innovative brain science to guide its product development to create the most effective learning and training solution, perfectly tailored to the way the human brain works. Learn more about how Amplifire helps people learn better and faster with online learning by requesting a demo.
-
Hacking the Forgetting Curve and the Clinical Implications of Forgetting
For many of us, forgetting something on the job isn’t a mortal mistake, but for healthcare professionals, one instance of forgetfulness can compromise a patient’s safety. Running a few minutes late to a meeting that slipped your mind doesn’t have the same fallout as a nurse forgetting to administer time-sensitive medication. There are many documented reasons as to why healthcare professionals may experience forgetfulness on the job. Clinician burnout is at an all-time high and stems from many causes, from frequent staff turnover to the exceptional emotional and physical demands of the job. There have been calls to action to improve patient safety systemically by developing standard care processes around common causes of patient harm and to align those processes with continuing education initiatives. But sometimes, it’s not the system that fails. It’s also not the burnt-out healthcare professional. It’s simply our biology: we forget things. But what if there were ways to forget less or remember more? In the high-stakes role of patient care, less forgetting can be the difference between life and death.
Why do we forget?
Although it may seem counterintuitive, there is actually a biological advantage to forgetting that is beneficial to humans’ overall cognitive abilities. Our brains are constantly processing and storing information, so it’s important to clear out unnecessary or irrelevant information to make room for new memories and learning. The forgetting process is crucial to our ability to adapt and respond to new experiences and can also help prevent overload and confusion in our brains. While the ability to remember anything and everything sounds good in theory, it is debilitating in reality. One famous example of such a condition is Solomon Shereshevsky, a Russian journalist who had an extraordinary memory, but also struggled with daily tasks due to his inability to forget irrelevant information. Shereshevsky was paralyzed by the constant flood of memories at the cue of even the most mundane stimuli. We’ve learned from Shereshevsky’s example that forgetfulness can be beneficial to our cognitive health by allowing us to filter out unnecessary information and focus on what’s important.
The Forgetting Curve
While forgetting is inevitable, that does not mean that we can’t understand how it works. Forgetting occurs at a generally fixed curve for all learned information. German psychologist Hermann Ebbinghaus first discovered the forgetting curve in 1885 while conducting a series of experiments on himself, where he memorized a list of nonsense syllables and then tested himself at various time intervals to measure how much he had forgotten. He found that there was a rapid decline in memory retention during the first hour after learning, with over half of the information forgotten within the first 20 minutes. The rate of forgetting slowed down after that, but there was still a significant decline over time. This curve is used throughout cognitive psychology to describe the natural rate of forgetting without any strategic intervention. As one can imagine, as humans with memories that can forget this quickly, this can have negative implications when training healthcare professionals on critical practices.

Clinical Implications of Forgetting
Forgetting healthcare training has serious clinical implications, particularly in the context of patient safety outcomes. Forgetting training can result in incorrect care or missed care, which can lead to patient harm. In a 2018 literature review of missed nursing care, clinical outcomes affected by missed care, as reported in nine studies, included: pressure ulcers, medication errors, nosocomial infections, patient falls, critical incidents, 30‐day hospital readmission and mortality.
Research on human error mechanisms suggested that, when highly trained, competent, well-intentioned human operators interact within complex systems, failures are inevitable. Trying to curb the inevitable process of forgetting with more training is fruitless if the training doesn’t stick. Ebbinghaus himself found that something as simple as incorporating repetition into learning can help flatten the forgetting curve. As it turns out, there are more strategies that can “hack” memory and prevent what we assume to be the inevitable process of forgetting.
Hacking the Forgetting Curve
The learning process is driven by the relationship between cause and effect. Causes out in the real world can lead to learning effects in the brain. In the cognitive science world, causes are known as “triggers” and the effects in the brain are known as “switches.” Some of the world’s most renowned cognitive scientists have identified which triggers are more conducive to faster, lasting learning compared to others. Some examples of triggers that flip memory-enhancing switches in the brain include repetition, spacing, and feedback. By incorporating these techniques into training strategies, retention greatly increases.

For example, incorporating spacing into learning can boost memory by 300% (Pashler, Rohrer, et al.). Research has shown that when restudy takes place too closely following the initial study session, there is little effect on memory. But it has also determined that the optimal study gap to test interval is 10% to 20% (ex: If the time to the test is 1 week, the optimal study gap between initial study and restudy is 1 day OR If the time to the test is 1 year, the optimal study gap is 3 weeks).
Another example is incorporating retrieval practice in the form of testing. In a study (Roediger and Karpicke) where groups of students were asked to 1) read a passage four times, 2) read the passage three times and test memory once, and 3) read a passage once and test memory three separate times, the third group that prioritized memory testing rather than only repetition retained 62% of the original information, whereas the first group retained just 39%. This demonstrates the power of activating the brain’s natural retrieval process to commit information strongly to memory. Learners can compound repetition and retrieval for better memory. Incorporating these strategies in training ensures that information sticks in the long run and is accessible in high-stress situations, like those experienced by healthcare professionals.
Despite the impressive effects of these memory “hacks”, we’re only human, after all, and forgetting will still happen — even to the most noble among us working in healthcare. However, in healthcare, forgetting can have serious clinical implications and compromise patient safety. The forgetting curve, discovered by Hermann Ebbinghaus, shows that forgetting occurs at a generally fixed rate for all learned information. To prevent forgetting and improve retention, training strategies should incorporate triggers like repetition, spacing, and feedback. By hacking the forgetting curve with training that sticks, we can ensure that healthcare professionals retain critical practices and reduce the likelihood of medical errors that can result in harm to patients.
From the beginning, Amplifire has relied on innovative brain science to guide its product development to create the most effective learning and training solution, perfectly tailored to the way the human brain works. Learn more about how Amplifire helps people learn better and faster with online learning by requesting a demo.
