-
Healthcare Course Catalog
Course content has been co-developed and efficacy-tested by co-development partners at renowned Health Systems across the country. Course content can be quickly deployed as is, or there are opportunities to develop new course content, supported by a dedicated content and design team.

-
Enhancing Patient Outcomes in Obstetrics Care: The Role of Quality Improvement
In recent years, maternal health in the United States has been declining. According to the Centers for Disease Control and Prevention, the maternal death rate in the US has risen steadily over the past decade, with the majority of these deaths being preventable. Combating this trend through quality improvement in obstetrics care has become a central focus. By implementing standardized care based on best practices and providing effective training, healthcare organizations have the power to significantly improve outcomes in obstetrics care and ensure patient safety.
The Impact of Quality Improvement
Quality improvement initiatives play a crucial role in achieving better patient outcomes in obstetrics care. Initiatives such as perinatal reviews and maternal quality collaboratives bring together healthcare providers from across the system to discuss and learn from cases of adverse outcomes, leading to performance improvement. Most healthcare organizations acquire international certifications, like the Joint Commission International Accreditation (JCIA), and accreditation of hospitals that recognize excellence in perinatal medicine. These initiatives ensure adherence to prescribed protocols and guidelines.
An example of standard care protocol success is a study on the California Maternal Quality Care Collaborative (CMQCC) Toolkit that provides approaches and strategies for providing care to women with maternal hemorrhage, hypertension, and severe sepsis. The implementation of this Toolkit averted 913 cases of severe maternal morbidity (SMM), 28 emergency hysterectomies, and one maternal death. It also resulted in $9 million saved.
The success of the Toolkit lies in its standardized, evidence-based protocols that greatly improve clinical management. “Quality improvement efforts in maternity care not only save lives; they can save costs,” said study co-author Elliott Main, MD, clinical professor of obstetrics and gynecology at Stanford Medicine and medical director of the California Maternal Quality Care Collaborative. Dollars saved can be reinvested into staff training to further improve maternal care and outcomes. For so many health systems that follow Joint Commission standards but still fall short of their patient safety goals, effective training is the link between having standards in place and ensuring standardized action and care. But implementing successful quality improvement training at scale can be challenging. Here are some critical points to consider.
Steps to successful quality improvement in obstetrics care
1. Utilizing the power of data analytics and technology
Obstetrics care also benefits significantly from data analytics and technology as the application of business intelligence systems can help monitor and analyze large volumes of data to identify likely adverse events. Predictive analytics can help detect early warning signs and intervene before an adverse event occurs. The use of electronic health records makes data recording, graphing, and analyzing easy, which can help identify deviations from standard care practices with ease. Technology also empowers patients to participate in their care plan by accessing data at any time and communicating with healthcare providers.
2. Reinforcing established standard practices with effective training
Establishing standard care processes, such as the Joint Commission’s, is just the beginning. It is equally important to ensure that these practices are understood, followed, and regularly updated. But simply offering training is not enough — clinicians need fast and effective training that works. Otherwise, the standard best practices health systems work so hard to identify and develop are useless. Continuous improvement of skills and knowledge, rigorous training exercises, and assessment can significantly enhance performance. By delivering safe and effective treatment during pregnancy, childbirth, and the postpartum period, healthcare providers can make a tangible difference in patient outcomes.
3. Prioritizing patient equity
Centers for Disease Control and Prevention (CDC) data reveals that American Indian/Alaska Native and Black women are 2 to 3 times as likely to die from a pregnancy-related cause than white women, among other figures that indicate racial disparities in obstetrics care and patient outcomes. Although this data created much-needed awareness around this issue, simply recognizing the problem does not translate to improved outcomes. Quality and improvement teams need clear action plans around this issue to be reinforced with effective training. Obstetrics departments that successfully tackle this gap in care will set themselves apart from those who do not make it a priority.
4. Emphasizing patient empowerment and informed consent
Patient empowerment is critical to enhancing obstetrics care outcomes and maximizing quality improvement efforts. Research indicates that patient education efforts have been proven to lead to more positive outcomes. Care goes beyond applying procedures or making a diagnosis. Patients and their families need to embody trust and collaborate in partnership with healthcare providers, enabling better decision making, and developing the understanding that supports shared goals and transparent communication. This way, patients are better empowered to make informed decisions about their care.
The declining maternal health statistics in the United States are alarming, and it is up to us as healthcare providers to adopt data-driven standardized care, reinforced by effective training, to enhance patient outcomes in obstetrics care. Implementing standard care practices, revisiting continuous learning and training, utilizing data analytics and technology, and empowering patients are just some of the critical elements that can be expanded upon to set the system on a positive trajectory. It is vital that those decision-makers who oversee care delivery invest in these strategies and make addressing the decline in maternal health statistics a priority. Ultimately, this will improve obstetrics care, increase maternal and infant safety, and empower women in their healthcare.
-
Why Effective Obstetrics Training Matters More Than Ever
Despite continuous medical advancement, the risk of maternal mortality and morbidity is increasing. The Center for Disease Control and Prevention data shows that the US maternal death rate rose sharply in 2021. This alarming figure follows in the wake of a global pandemic, where caution and safety were at the forefront of clinicians’ minds. Moreover, while maternal mortality rates have decreased 43 percent, globally, since 1990, the US is the only developed country where it has increased. The problem only becomes graver from a demographic perspective, where American Indian/Alaska Native and Black women are 2 to 3 times as likely to die from a pregnancy-related cause than white women.
Why is the US trailing behind other developed countries when it comes to maternal health? In a time where clinician burnout is rising and organizations face high turnover rates, the US not only saw maternal health decline, but patient safety as a whole. A 2022 literature review by senior leaders in health systems directly dealing with patient safety issues, stated that “Patient safety policy and practice has relied too heavily on the vigilance and heroism of clinicians, rather than the design of safe systems.” And in response to recent patient safety declines, they propose proven-effective training combined with standardized care processes to improve outcomes.
Now, more than ever, health systems need obstetrics training they can trust; meaning, training that works. In the new age of online learning, it can be difficult to distinguish between what works and what doesn’t, and what meets high-performing health systems’ standards, and what falls short. Here’s what to look for in an online learning platform for obstetrics training.
-
The Essential Obstetrics Checklist: 8 Must-haves to make your OB training a success
Despite continuous medical advancement, the risk of maternal mortality and morbidity is increasing. The Center for Disease Control and Prevention data shows that the US maternal death rate rose sharply in 2021. Now, more than ever, health systems need obstetrics training they can trust; meaning, training that works. In the new age of online learning, it can be difficult to distinguish between what works and what doesn’t, and what meets high-performing health systems’ standards, and what falls short. Here’s what to look for in an online learning platform for obstetrics training.
-
Knowledge variation in OB creates risk
Childbirth is a natural process that usually ends with a healthy mother and baby. But severe complications can occur suddenly that require a quick, accurate response. When things go wrong in obstetrics, the reasons are often unclear, but a lack of knowledge is frequently the root cause. Errors in clinical judgment were cited in 77% of more than 800 clinically coded obstetric malpractice cases according to CRICO Strategies, which offers clinical risk intelligence to 400+ hospitals and more than 180,000 physicians.
This study aims to show the hidden variation in the knowledge that may lead to errors during childbirth. It used the Amplifire learning platform, which is based in cognitive science and proven in over three billion learner interactions.
Study Design
310 Nurses and 192 Providers Patient-facing OB nurses and OB doctors at a large east coast hospital received four Amplifire courses covering critical aspects of obstetrics:
• Reduce incidents and near-misses associated with the health and safety of pregnant women and their unborn children
• Reduce the financial burden of malpractice claims associated with obstetrics
• Address the most frequently seen rule-based, skill-based, and knowledge-based active and latent errors in obstetrics
• Target and reduce the most common system errors related to electronic fetal monitoring (EFM) including fear of conflict, knowledge deficits, and communication failures
By the end of each course, 100% of the clinicians were proficient (confident and correct) on all the material.
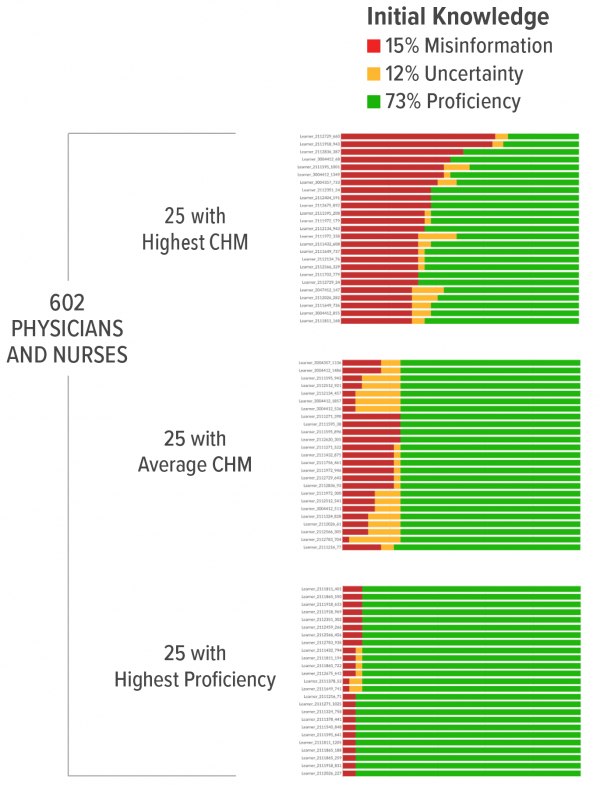
Electronic Fetal Monitoring
This heatmap is taken from Amplifire’s reporting dashboard and shows the clinicians sorted by their amounts of confidently held misinformation, uncertainty, and proficiency.
- 654 clinicians generated 13,080 data points
- 3,121 instances of confidently held misinformation were corrected
- 2,672 instances of uncertainty were corrected
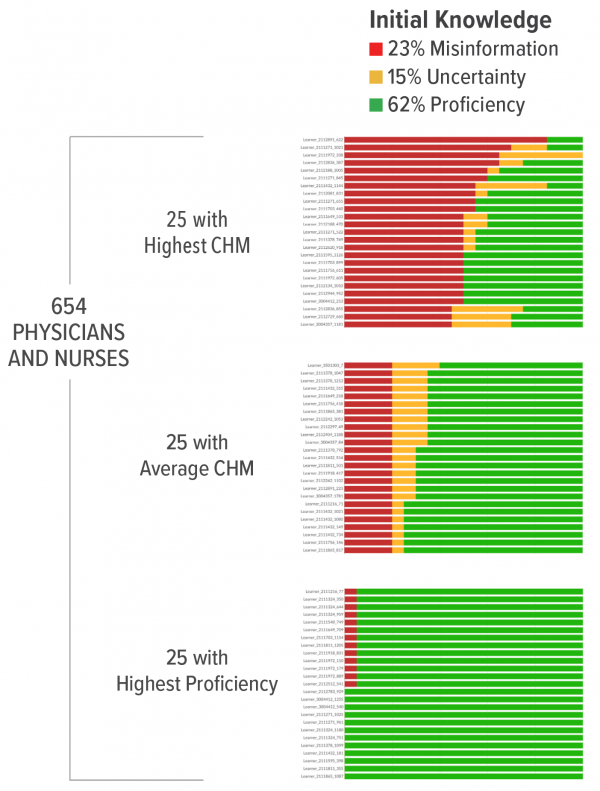
Postpartum Hemorrhage
- 654 clinicians generated 13,080 data points
- 3,008 instances of confidently held misinformation were corrected
- 1,962 instances of uncertainty were corrected
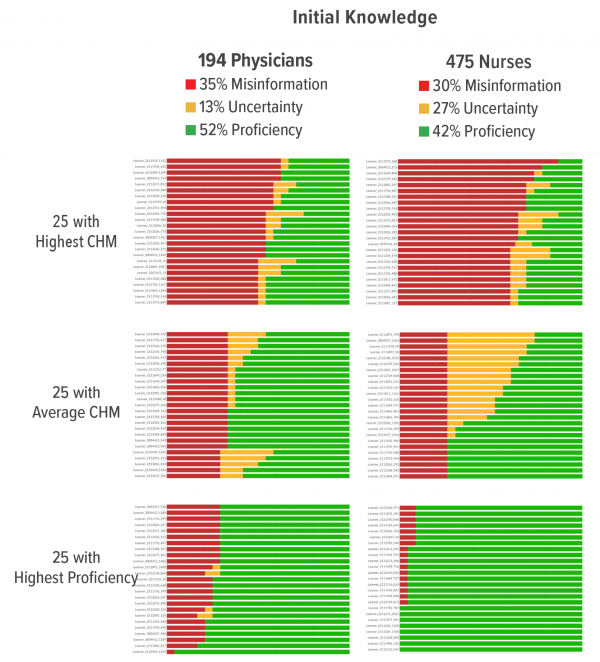
Hypertension in Pregnancy
- 194 physicians and 475 nurses generated 4,462 data points
- 4,838 instances of confidently held misinformation were corrected
- 3,529 instances of uncertainty were corrected
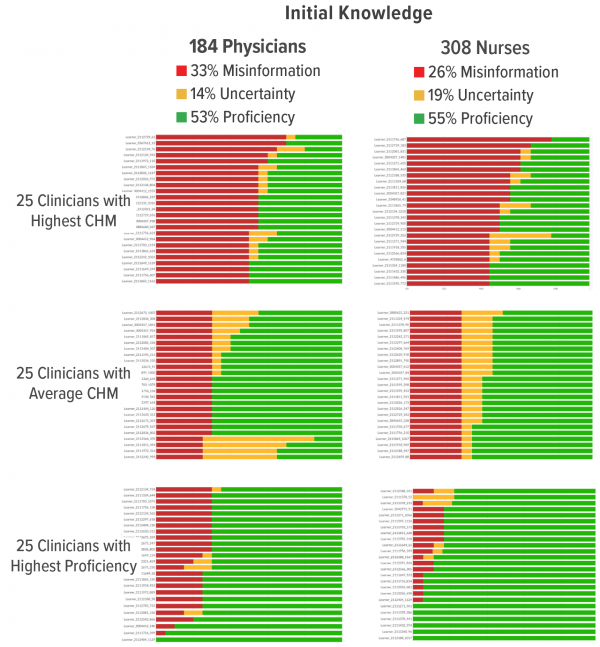
Shoulder Dystocia
- 184 physicians and 308 nurses generated 9,348 data points
- 2,674 instances of confidently held misinformation were corrected
- 3,122 instances of uncertainty were corrected
Clinical Implications
Download the full case study to see all of the findings and clinical implications.
