-
CLABSI study – A new Pathway to Reduce CLABSI in hospitals
CLABSI Study – A New Pathway to Reduce CLABSI in Hospitals
Central venous catheters (CVCs) are used for the administration of intravenous fluids, blood products, medications, and parenteral nutrition. They also provide access for hemodialysis and other forms of long-term treatment, such as chemotherapy.
Widespread and essential, CVCs are also a frequent cause of healthcare-associated bloodstream infections. It is estimated that 250,000 cases of central line–associated bloodstream infections (CLABSIs) occur in the U.S. every year. According to the CDC, CLABSIs are associated with a mortality rate of 12–25%. Each CLABSI episode costs approximately $22,000, which includes the burdens of additional diagnosis and treatment, and prolonged hospital stays.
CLABSI rates can be reduced, if not eliminated, by adherence to evidence-based protocols. National CLABSI rates have shown a 50% drop between 2008 and 2016. Several hospitals throughout the U.S. have managed to maintain a 0% CLABSI rate for months, even years, by following these protocols.
So why does CLABSI still happen? A major US health system employed the Amplifire training tool to acquire data on what its nurses know and don’t know about these protocols for managing CVCs, and to find and fix any misinformation the nurses held.
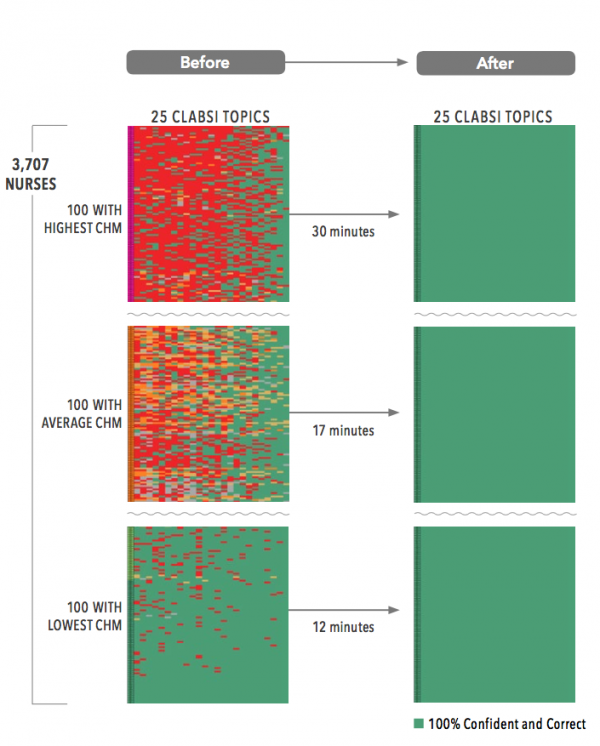
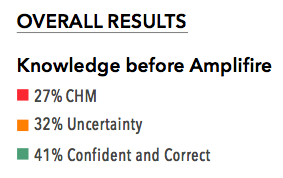
Knowledge and Confidence About CLABSI Before and After Amplifire
Observations
- 25,129 instances of CHM found and fixed
- 29,838 instances of uncertainty found and fixed
- The variation of knowledge was high, with some nurses quite misinformed and others showing confident mastery of the topic. The most knowledgeable were 100% confident and correct about CLABSI. The least show that misinformation occupied up to 60% percent of their knowledge.
- Nurses who were most misinformed or uncertain spent nearly a half hour in the module, whereas nurses who were most knowledgeable about CLABSI spent only 12 minutes.
- By the end of the course, 100% of the nurses who completed were confident and correct on all the information.
-
Fixing misinformation to reduce Sepsis risk
A New Pathway to Reduce Sepsis Morbidity
Every hour that a sepsis diagnosis is missed, mortality increases 8%. In recent years, the scale of the problem has driven new, international efforts to improve sepsis care. No specialty “owns” sepsis. It’s all hands on deck. There are newly devised protocols, sepsis teams, guidelines, and alliances to combat sepsis. Providers, payers, researchers, risk underwriters, accreditors, and regulators are all on notice to reduce sepsis morbidity and mortality.
There are isolated, local successes. Intermountain Healthcare in Salt Lake City reduced sepsis mortality by 70% through innovation and organizational grit…and knowledge.
First-of-its-kind national hospitalist sepsis study
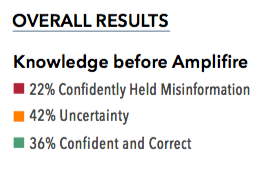
Our first-of-its-kind national hospitalist sepsis study was designed as a clinical intervention using the Amplifire training tool, which delivers a groundbreaking learning experience and advanced analytics. The goal was to acquire data on what doctors and nurses know about sepsis. Can they recognize sepsis at an early stage? Do they know the evidence supporting treatment guidelines? Are they confident about how to respond?
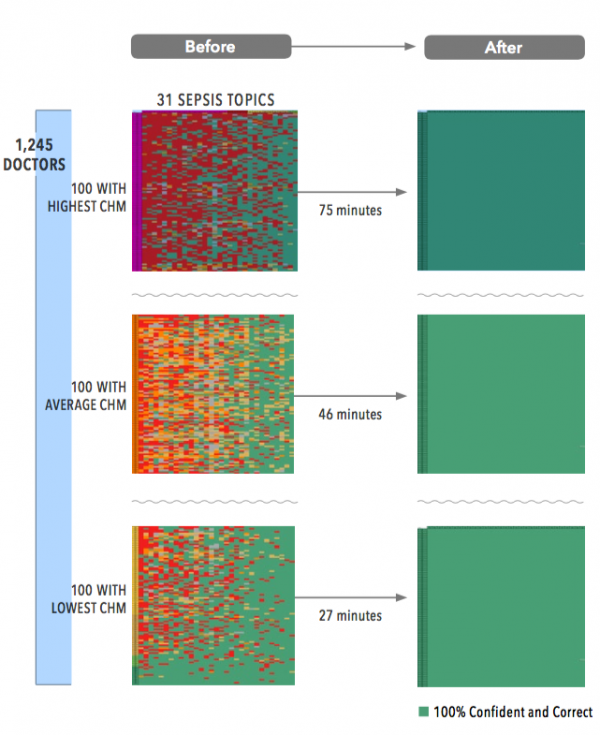
Finding and Fixing Confidently Held Misinformation (CHM) that Affects Performance
Observations
- 7,795 instances of confidently held misinformation found and fixed
- 14,500 instances of uncertainty found and fixed
- The variation of knowledge was high, with some doctors misinformed and others showing con dent mastery of the topic. The most knowledgeable are nearly 100 percent confident and correct about sepsis. The least knowledgeable revealed misinformation about more than half the topics
- Doctors who were most misinformed or uncertain spent well over an hour in the module, while those who already knew much about sepsis spent only 27 minutes
- By the end of the course, 100% of the clinicians who completed were confident and correct on all the information
Clinical Challenges and Implications
Amplifire discovered that there was a lot of confusion around source awareness, age bias and guidelines.
-
Uncertainty and Variation in Clinician Knowledge About Sepsis
A Pattern We Have Never Seen: An Extraordinary Amount of Uncertainty
Amplifire has measured certainty through nearly a billion learner interactions over the last decade. What we’ve never seen before is high uncertainty among clinicians. Usually, doctors are confident in what they think they know, but in our latest sepsis pilot, doctors had high levels of uncertainty regarding new information about sepsis.
The sepsis course was designed around the latest evidence-based data, practices, and bundles in recognizing and treating sepsis. The doctors perceived correctly that this was new information for them and were honest about their uncertainty.
Human beings are predisposed to overconfidence because it’s an adaptive feature that was forged in human psychology. Confidence is an attractive trait that has led to survival and success for those who display it proudly, even when that confidence is sometimes misplaced. It is difficult for most professionals to acknowledge their uncertainty, even when it is warranted. Not so with these docs.
Visualizing Clinician Variation
Doctors need the freedom to exercise their decision-making powers in the face of human complexity. However, doctors should not be making decisions based on out-of-date information. Old information that gets welded into memory in medical school is hard to identify and harder to eliminate. Continuing medical education has no ability to identify this confidently held misinformation (CHM), much less eliminate it.
The wide range of doctor experience since medical school is what we are seeing when we look at the variation among doctors seen below. The graph shows the range of confidence and accuracy for three doctors pulled from the best, average, and worst ends of the heatmap.
-
Physicians, Sepsis, and Cognitive Dissonance Early Diagnosis & Treatment of Sepsis
The Annals of Emergency Medicine recently published a paper entitled “Preliminary Performance on the New CMS Sepsis-1 National Quality Measure: Early Insights From the Emergency Quality Network (E-QUAL).” In the paper, the authors review the performance of hospitals against the CMS Severe Sepsis/Septic Shock Early Management Bundle (SEP-1) quality measure. Their conclusion is that “preliminary data on SEP-1 performance suggest wide hospital-level variation in performance, with modest improvement during the first year of data collection.”
Within that conclusion lies perhaps the greatest tension underlying the herculean efforts to make healthcare better, safer, and more affordable. This tension is whether patients get the right care, better care, and cheaper care if clinical decisions are codified, governed, or even digitized, according to evidence, best practice, and guidelines. Or, is the right care, better care, and cheaper care better off in the hands of physicians to use their knowledge, experience, and judgment, with evidence, best practice and guidelines only used as a reference?
Stated differently, it’s the ongoing ideological war over what some people call “Cookbook Medicine.” Those who govern healthcare want to create approved recipes for clinical care that doctors follow. The assumption is that those recipes are the best possible recipes and consistently result in the best results for most patients, regardless of who and where they are. With physicians, this assumption causes cognitive dissonance.
This dissonance starts, according to sepsis specialist Dan Davis, MD, Director of the Center for Resuscitation Science at the University of California, San Diego (UCSD), “When regulatory requirements parallel clinical guidelines that appear somewhat arbitrary and capricious. There is no better example than the sepsis guidelines, which have been inconsistent at best, and outright contradictory at worst. And yet they influence hospital performance metrics and reimbursement. Cognitive dissonance manifests quite impressively in the physician approach to mandatory education. Once the information is perceived as having regulatory (but not clinical) relevance, the approach becomes pragmatic, and the learned information is laid down with less permanence and without connection to clinical practice neural networks (which involve both right and left brain connections).”
The SEP-1 data, which drew from chart review at 50 emergency departments across the US, did not investigate sepsis outcomes; it measured compliance with the SEP-1 bundle. The fact that variation was wide and performance only modestly improved suggests that physicians and their hospitals:
- Don’t know the SEP-1 bundle
- Have difficulty interpreting and/or applying it
- Follow a different set of guidelines or practices
- Disagree with the evidence behind SEP-1
- And/or simply forgot to document or report their compliance
Sepsis has been around for a long time, as has the lack of agreed-upon knowledge about the best way to recognize and treat it. As physicians and standard-setters hold their ground, patients continue to suffer.
But there is hope.
The Amplifire Healthcare Alliance recently completed a national multi-site sepsis study involving 1,234 hospitalists, ER physicians, CCU physicians, and nurse practitioners across 23 hospitals and health systems. All study participants took the same accredited 30-minute sepsis course deployed on the Amplifire platform. The course included the most current evidence for diagnosing and treating sepsis and was vetted by the internal sepsis leaders at all 23 participating organizations.
While the findings of the Alliance study were startling — showing a great deal of confidently held misinformation and uncertainty among practicing clinicians about their understanding of the evidence for sepsis care—they were not surprising given the SEP-1 study findings. The Alliance study also revealed that Amplifire may represent a scalable way for hospital executives to reduce the cognitive dissonance physicians have toward sepsis (and other) evidence and guidelines, and thereby reduce clinical variation and increase guideline adherence.
