-
What in the World is Confidently Held Misinformation?
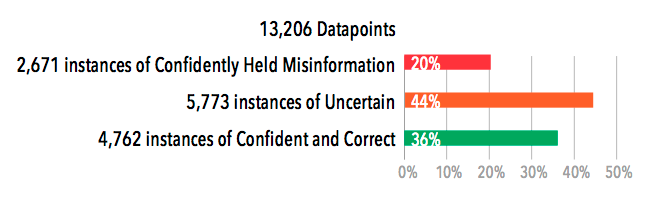
Confidently held misinformation (CHM), refers to misinformation that is relied on as if it were true. Our clients have found an average of 25 – 35% false confidence within their organizations. This indicates that within their workforce, almost a third of employees’ knowledge is unknowingly incorrect — which opens the door to risk, harm, and loss for both themselves and their clients.
Risk that most organizations encounter stems from decisions to act based on misinformation disguised as truth. The graph below shows the amount of CHM we have uncovered throughout various industries and among thousands of working professionals — from doctors to pilots to satellite TV technicians. Notice that the level of false confidence is similar across industries. Everyone is susceptible to CHM.

Confidently held misinformation has brought down businesses, changed lives, and affected innocent bystanders. What harm could CHM do to your organization?
“It’s not what you don’t know that will hurt you. It’s what you think you know that just ain’t so.”
Mark Twain
-
Curiosity Accelerates Mastery
The remarkable feline brain has been programmed by roughly 30 million years of evolution into that of a dogged information gatherer and pattern recognizer. Cats are the epitome of curiosity and what they accomplish during their daily explorations is really knowledge mastery.
Think about this little Russian Blue for a moment. Like all cats, she spends a part of every day on the prowl. The vast array of information that she seeks and obtains through the motivating power of curiosity gives her a near-perfect map of the property she inhabits and controls—a confident and correct sense of who is friend, foe, or food. And she updates her knowledge whenever doubt and uncertainty creep in. The famous curiosity of cats is really that updating process made plain. Move a chair in the living room or rearrange the garden, and she immediately realizes the map in her head is not the same as the data now streaming in for comparison.
Knowledge is vital and she is unremitting in its accurate acquisition. She is especially attuned to what psychologists call an information gap. When something changes, our cat quickly sets about exploring the altered landscape and recreating a new map that is confidently navigable for pursuing prey or escaping predators. She closes the information gap. Doubt is banished and mastery is attained. It’s a matter of life and death for her, so she strives to master knowledge because it vastly improves the chances of mastering her fate.
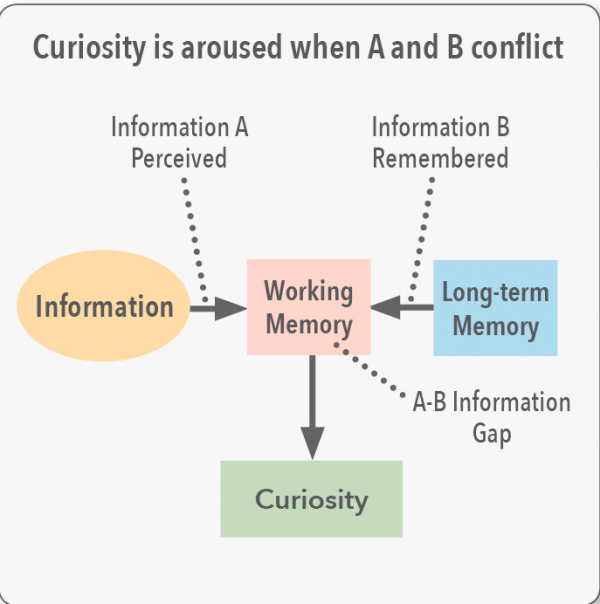
This, in fact, may be the biological source of uncertainty in all mammals including the human variety. Uncertainty is felt when sensory information about the terrain, an idea, or a face is held in working memory, but it does not correspond with the patterns being pulled in from long-term memory. As shown in the illustration at right, it is this conflict that produces the information gap that leads to both uncertainty and curiosity.
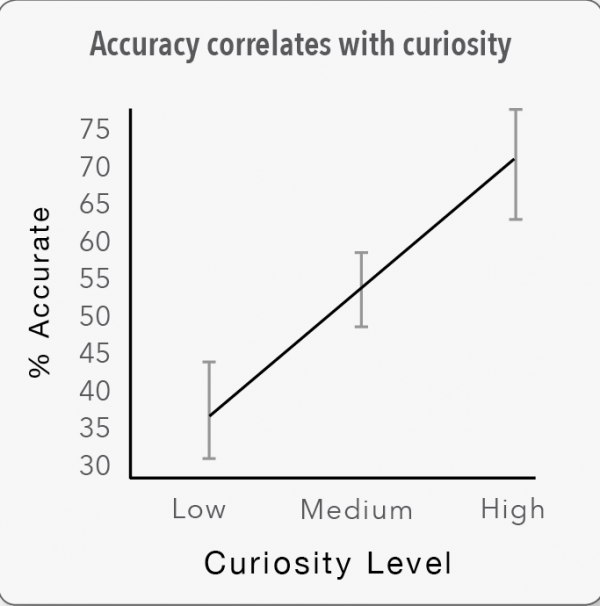
In psychological experiments, the effect of curiosity on student performance is profound. In a set of studies that looked at both the underlying physical circuitry involved in curiosity (prefrontal cortex, caudate, hippocampus, etc.) and its empirical effect on memory, Kang, et al., found a direct correlation with learning.
“Curiosity showed a strong effect on subsequent recall of the answers to the questions that were initially guessed incorrectly…Consistent with the fMRI findings, these findings suggest that curiosity activates memory regions differently in response to surprising (incorrectly guessed) answers.”
For good reason, the provocative title of Kang’s research paper on the motive power of curiosity is “The Wick in the Candle of Learning.” As Kang notes, people in the education industry would do well to figure out how to prime students’ hunger for knowledge using small amounts of information tinged with uncertainty.
-
Uncertainty and Variation in Clinician Knowledge About Sepsis
A Pattern We Have Never Seen: An Extraordinary Amount of Uncertainty
Amplifire has measured certainty through nearly a billion learner interactions over the last decade. What we’ve never seen before is high uncertainty among clinicians. Usually, doctors are confident in what they think they know, but in our latest sepsis pilot, doctors had high levels of uncertainty regarding new information about sepsis.
The sepsis course was designed around the latest evidence-based data, practices, and bundles in recognizing and treating sepsis. The doctors perceived correctly that this was new information for them and were honest about their uncertainty.
Human beings are predisposed to overconfidence because it’s an adaptive feature that was forged in human psychology. Confidence is an attractive trait that has led to survival and success for those who display it proudly, even when that confidence is sometimes misplaced. It is difficult for most professionals to acknowledge their uncertainty, even when it is warranted. Not so with these docs.
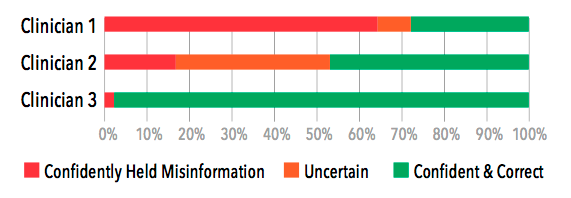
Visualizing Clinician Variation
Doctors need the freedom to exercise their decision-making powers in the face of human complexity. However, doctors should not be making decisions based on out-of-date information. Old information that gets welded into memory in medical school is hard to identify and harder to eliminate. Continuing medical education has no ability to identify this confidently held misinformation (CHM), much less eliminate it.
The wide range of doctor experience since medical school is what we are seeing when we look at the variation among doctors seen below. The graph shows the range of confidence and accuracy for three doctors pulled from the best, average, and worst ends of the heatmap.
-
Physicians, Sepsis, and Cognitive Dissonance Early Diagnosis & Treatment of Sepsis
The Annals of Emergency Medicine recently published a paper entitled “Preliminary Performance on the New CMS Sepsis-1 National Quality Measure: Early Insights From the Emergency Quality Network (E-QUAL).” In the paper, the authors review the performance of hospitals against the CMS Severe Sepsis/Septic Shock Early Management Bundle (SEP-1) quality measure. Their conclusion is that “preliminary data on SEP-1 performance suggest wide hospital-level variation in performance, with modest improvement during the first year of data collection.”
Within that conclusion lies perhaps the greatest tension underlying the herculean efforts to make healthcare better, safer, and more affordable. This tension is whether patients get the right care, better care, and cheaper care if clinical decisions are codified, governed, or even digitized, according to evidence, best practice, and guidelines. Or, is the right care, better care, and cheaper care better off in the hands of physicians to use their knowledge, experience, and judgment, with evidence, best practice and guidelines only used as a reference?
Stated differently, it’s the ongoing ideological war over what some people call “Cookbook Medicine.” Those who govern healthcare want to create approved recipes for clinical care that doctors follow. The assumption is that those recipes are the best possible recipes and consistently result in the best results for most patients, regardless of who and where they are. With physicians, this assumption causes cognitive dissonance.
This dissonance starts, according to sepsis specialist Dan Davis, MD, Director of the Center for Resuscitation Science at the University of California, San Diego (UCSD), “When regulatory requirements parallel clinical guidelines that appear somewhat arbitrary and capricious. There is no better example than the sepsis guidelines, which have been inconsistent at best, and outright contradictory at worst. And yet they influence hospital performance metrics and reimbursement. Cognitive dissonance manifests quite impressively in the physician approach to mandatory education. Once the information is perceived as having regulatory (but not clinical) relevance, the approach becomes pragmatic, and the learned information is laid down with less permanence and without connection to clinical practice neural networks (which involve both right and left brain connections).”
The SEP-1 data, which drew from chart review at 50 emergency departments across the US, did not investigate sepsis outcomes; it measured compliance with the SEP-1 bundle. The fact that variation was wide and performance only modestly improved suggests that physicians and their hospitals:
- Don’t know the SEP-1 bundle
- Have difficulty interpreting and/or applying it
- Follow a different set of guidelines or practices
- Disagree with the evidence behind SEP-1
- And/or simply forgot to document or report their compliance
Sepsis has been around for a long time, as has the lack of agreed-upon knowledge about the best way to recognize and treat it. As physicians and standard-setters hold their ground, patients continue to suffer.
But there is hope.
The Amplifire Healthcare Alliance recently completed a national multi-site sepsis study involving 1,234 hospitalists, ER physicians, CCU physicians, and nurse practitioners across 23 hospitals and health systems. All study participants took the same accredited 30-minute sepsis course deployed on the Amplifire platform. The course included the most current evidence for diagnosing and treating sepsis and was vetted by the internal sepsis leaders at all 23 participating organizations.
While the findings of the Alliance study were startling — showing a great deal of confidently held misinformation and uncertainty among practicing clinicians about their understanding of the evidence for sepsis care—they were not surprising given the SEP-1 study findings. The Alliance study also revealed that Amplifire may represent a scalable way for hospital executives to reduce the cognitive dissonance physicians have toward sepsis (and other) evidence and guidelines, and thereby reduce clinical variation and increase guideline adherence.
-
Is Medical Simulation the Answer to Patient Safety?
Medical errors stubbornly remain the third-leading cause of death in the U.S. Although medical institutions are investing in new patient safety training, it has not been enough to put a dent in this global problem.
Why is this and what can be done?
Cognitive Learning Behavior
A big part of the problem lies in the fact that traditional classroom training, while inexpensive, is only partially effective because learners will forget 75% of the material in about a week.
Traditional teaching methods employ passive forms of learning, such as lectures and reading. Neuroscientists have found that humans learn more and retain information longer when active and varied learning techniques are used. When learning is made harder, knowledge sticks. (Henry Roediger, author of Make It Stick).
Learning on The Job
Healthcare professionals are expected to take what they have learned in the classroom and apply it on the job. While this practice is common in most professions, in healthcare, the stakes are simply too high.
Healthcare professionals need a safe learning environment to practice and perfect their technique. Simulation-based training seems to be the answer.
Simulation-based Training
Medical simulation training has proven to be 95% effective. Meaning only 5% of the knowledge is forgotten. Simulation-based training gives medical students the opportunity to repeatedly practice a technique until they have mastered it.
“Training that simulates the kinds of demands and changeable conditions that can be expected in real-world settings help learners and trainers assess mastery and focus on areas where understanding and competency need to be raised”, says Roediger.
The benefits of medical simulation-based training are indisputable. In an ideal world, all healthcare providers would experience hands-on training before practicing on an actual patient.
The University of Tennessee Health Science Center has invested in a new a $37 million medical simulation facility opening in the fall. It will house exam rooms, hospital beds, operating tables, residential settings, and even a pharmacy where medical students will receive hands-on training.
Why aren’t more healthcare systems and medical teaching facilities quickly adopting this methodology? Look at that price tag – $37 million.
Healthcare Training Needs to Be Scalable and Affordable
Medical simulation facilities and programs are cost-prohibitive for many medical institutions, yet to significantly reduce medical error, an alternative training solution must be found that is:
- Affordable and scalable.
- Grounded in research on learning behavior.
- Efficient so that healthcare providers spend less time in the classroom and more time on the floor.
An Innovative Approach to Medical Training
Amplifire has developed new ways of measuring knowledge acquisition, content mastery, and retention. Amplifire’s learning management system is different from any other because it:
- Primes the mind for learning using the cognitive technique known as retrieval
- Creates confidence-based questions stimulate focus, thinking, and memory.
- Spotlights risks for the learner and the organization. Through data analytics and heatmap reporting, risks that can lead to poor outcomes are identified and listed by topic, department, or individual.
- Personalizes training, making it less time consuming.
- Presents learners with timely refreshers on the content they are most likely to forget.
The Solution to Improving Patient Safety
There is no one solution to improving patient safety. It will take a combination of training techniques and tools to solve this global healthcare problem. But a learning approach that is scalable and affordable will help healthcare systems move the needle in reducing avoidable patient harm.
-
Is Your LMS Underperforming For Your Healthcare System?
Transforming Healthcare Training
Despite all of the time and money spent on healthcare training, it can be ineffective, a waste of time, not memorable, and create an illusion of knowledge where none may exist.
But it doesn’t have to be.
There are new learning technologies that make knowledge stick and easier to recall. Learning systems that eliminate misinformation that leads to patient harm.
Take our quiz below and see how well your LMS system is performing.
Quiz:
- Does your LMS contain analytics demonstrating clinician learning gains?
- Does your current LMS tell you specifically which of your physicians and nurses carry inaccurate information or maintain incorrect practices that pose risks to patients?
- Does your LMS validate each learner’s mastery of a topic and monitor, maintain and report on their knowledge over time?
- Does your current LMS provide ROI projections and measure efficacy on the courses it delivers?
- Which of the following statements best describes your current LMS (choose one):
a. Our LMS is a human resource system that monitors the completion of mandatory training by staff.
b. Our LMS provides our learners with a broad range of clinical and non-clinical courses to maintain their competency and track their completion of mandatory training.
c. Our LMS is driven by organizational performance goals and provides evidence of physician and staff knowledge and actionable data to managers to help their physicians and staff deliver on those performance goals.
Results:
If you answered “no” to any questions 1-4, or answered (a) or (b) to question 5, your LMS is underperforming.
-
Amplifire Heatmaps – A Quick Orientation
You can think of the heatmap as a visual proxy for the pattern of neurons that represent information in the minds of clinicians. Furthermore, think of confidence as the precursor to the decision making that leads to behavior. When you are confident, you act. When you are confident yet wrong, a mistake becomes far more likely.
The Amplifire algorithm is based in the cognitive psychology of learning and memory and adapts to each learner. If a learner is confident and correct on a question, they never see it again. If they are confident and wrong, the system will show them concise explanations and ask them the question again later in the module. Everyone gets to confident and correct along their own unique path.
After Amplifire
The algorithm does not allow a learner to escape until all confidently held misinformation and uncertainty are eliminated. The heatmap on the right represents a state of mastery. Is it permanent? Sadly, no.
CHM is made up of neurons that are connected in a strong pattern, and this pattern will return. Regression is a topic we consider elsewhere, but suffice to say that our analysis of over a million learners in Amplifire indicates that about 75% CHM is permanently eliminated but 25% CHM returns within a month. Amplifire refreshers are designed to reduce regression over time. CHM can be tamed, but the brain’s architecture and processes mean that a 100% instantaneous fix does not appear possible.
Despite this reality, 100% confident and correct across all topics is indeed possible, as we regularly see that state in our refresher heatmaps. Like most things, it just takes some work to get there.
-
A Primal Scream for Evidence-based Medicine
More than anything, physicians want clarity. They want to be empowered to make evidence-based decisions that lead to the best possible patient outcomes.
When physicians scream for more evidence-based medicine, they’re really screaming for involvement. They want a say in the content of their training – will it focus on guidelines, and if so, will those guidelines align with evidence?
You want to help them, but so far, your training options have been limited. You’ve found that superficial training simply doesn’t elicit enthusiasm or buy-in.
Helping physicians means implementing a training program that gives them a voice. You need an evidence engine that involves physicians in the process of finding and fixing confusion.
The Future of Evidence-based Medicine
The Institute of Medicine said 90% of medical decisions will be based on evidence by the year 2020. This is based on the assumption that medical evidence will become increasingly available, shared, and understood. Policymakers, payers, hospitals, doctors, nurses, and patients will need to join together to rein in the evidence and use it as a weapon for harmony.
Finding and Fixing Confusion
We share your passion for evidence and physician involvement. That’s why we developed a method of mapping physician knowledge that doesn’t point fingers, but leads to discussion.
Amplifire is an evidence-based learning platform that aims to reduce clinical variation without forcing physicians to follow protocols they don’t believe are evidence-based.
Detailed learning data ensures that hospitals and healthcare systems take seriously the input and evidence from physicians, and use it to arrive at evidence-based practices embraced by all.
-
Hospitalists: A New Way to Measure Healthcare Quality
Over 40 years ago, at the start of my healthcare career, I was introduced to the Donabedian Model for healthcare quality. We all are familiar with this conceptual framework, consisting of three fundamental elements defining quality:
- Structure
- Process
- Outcomes
Donabedian Model:
Today, the Donabedian Model is embedded in the American healthcare system. Medicare’s quality metrics are categorized and measured as either Structure, Process, or Outcomes. To use a cooking metaphor:
- Structure consists of the ingredients and the equipment.
- Process consists of the recipe.
- Outcomes measure quality – does it taste good?
Cognitive Learning Behavior
For the most part, the way we learn has remained unchanged for centuries. Students study and then take an exam to measure what they’ve learned. And then a lot of that learned knowledge is forgotten.
Amplifire, a “knowledge engineering” platform, focuses on human learning behavior.
Technology has been used to improve the “packaging” of content being taught. While these innovations have made it easier for the teacher to teach, it hasn’t done much to help learners learn.
The cognitive science experts behind Amplifire have tackled this challenge head on. Over the past 30 years, as a result of substantial advancements in the field of brain science, we now know a great deal about how the brain encodes, stores, and retrieves information. Amplifire has incorporated these techniques into its software algorithm and demonstrated superior results in many knowledge domains, including aviation, manufacturing, and higher education.
So what does this have to do with the Donabedian Model?
I can make the case that in addition to Structure, Process, and Outcomes, KNOWLEDGE may be the fourth element of healthcare quality. Let me use the cooking metaphor again. If Julia Child and I were both cooking the same roasted chicken, and we both had the same ingredients, equipment, and recipe, her chicken would undoubtedly taste better than mine. Why? Because she has superior KNOWLEDGE, where knowledge is defined as the integration of learned information and practical experience.
Re-engineering Healthcare
As we attempt to re-engineer healthcare and improve quality by increasing the use of evidence-based practices, very little is being done to help clinicians improve how they learn and gain knowledge.
There are occasional workshops and e-learning modules. But most efforts today are directed towards using the electronic medical records (EMR) to standardize workflows, implement alerts, and provide automated decision support.
Ironically, these efforts are directed towards creating fail-safe processes that do not depend on clinician knowledge. (By the way, clinician education is still flourishing. But its focus is less on knowledge acquisition and retention and more on verifying that clinicians have taken the specified courses to meet board certification, licensure, and regulatory requirements.)
Knowledge Acquisition and Retention
Amplifire has made a major contribution to healthcare quality by developing new ways to measure knowledge acquisition, mastery, and retention. For example, it uses colorful, adaptive heatmaps to display existing and then eradicate Confidently Held Misinformation (CHM) – those hidden untruths in the minds of your clinicians that lead to harm and loss.
With clinician-specific data, this provides a powerful new platform to engage clinicians in quality improvement. At the same time, the platform can reveal and illustrate to clinical executives exactly where there are barriers are to moving the needle on mission-critical quality metrics.
Healthcare Alliance
In the last 18 months, Amplifire has targeted healthcare as the industry that is the best match for its capabilities. The company is developing a Healthcare Alliance, engaging healthcare organizations as strategic partners, using data and collaboration to support clinicians in improved learning.
Furthermore, Amplifire recognizes that hospitalists are THE critical physicians involved in healthcare transformation. As the former Senior Vice President for the Society of Hospital Medicine (SHM), I am a passionate supporter of hospital medicine, the fastest growing specialty in the history of medicine. As I learned about Amplifire, I recognized that it is a tool that can support hospitalists in their efforts to improve quality, safety, and patient experience. I am working with the company to educate hospitalists about the power of this knowledge engineering platform.
Hospitalist Pilot Study
A recent Hospitalist Pilot Study conducted by Amplifire focused on a mixture of clinical content, patient safety, and administrative content. The results indicated that learners knew (with confidence) 50% of the material. However, 32% of the content represented Confidently Held Misinformation (CHM). Over 69% of learners indicated they preferred Amplifire’s educational experience.
Knowledge Engineering Solutions
It may be audacious to suggest KNOWLEDGE as a fourth element to the Donabedian Model, a paradigm that has a sacred place in the healthcare industry. Perhaps KNOWLEDGE transcends or integrates the other three elements.
In any case, there is no doubt that improving hospitalist knowledge has the potential to improve healthcare quality.
Specifically, the study of 1,984 patients admitted to hospitals between 2008-2012 found that patients admitted during an unannounced Joint Commission survey had lower 30-day mortality rates than those patients admitted three weeks before or after the unannounced survey. The JAMA study’s authors said the most probable reason for the decrease in mortality during survey weeks is the “heightened scrutiny during visits” and the physical presence of surveyors, similar to how the Hawthorne effect contributes to better hand hygiene compliance.
Why is this study important? At first glance, it looks like it touts The Joint Commission as the long arm of the law and that hospital staff fall in line and take the best care of patients when being off their game could get them in trouble. In other words, the fear inspired by Joint Commission surveyors brings out the best in hospital staff.
Really? So what are we to do with this finding? Are we to extend greater superpowers to The Joint Commission to instill more fear, more continuously in hospital staff so that patients are safer? To do so would require a constant TJC presence in hospitals. How is that possible? More surveyors? More frequent unannounced surveyors, or 24/7 drone surveying? Deputized hospital staff to serve as whistleblowers? More real-time access to quality and safety data by TJC to monitor when things may be going wrong and swoop in with tasers?
The abiding question is whether fear is a sustainable motivator for performance. This study would suggest that fear works. But if you’re like me, when I’m in a state of fear, I seek the comfort of authority, I don’t trust my own judgment, I don’t use my peripheral vision, and I get frustrated by the sense of oppression. So, the REAL question from this study isn’t how we get more Joint Commission in healthcare; it’s how do we liberate healthcare from The Joint Commission to perform well without fear.
An antonym of fear is confidence. Today’s physicians and healthcare professionals have every reason to be afraid and every reason to lack confidence. Every decision made for patients is scrutinized by payers, regulators, and risk underwriters, with harsh consequences. Professional judgment is being codified into guidelines and standards of care because rogue physicians may go “off book” when caring for patients. Metrics are imposed on physicians that are supposed to represent “quality”, and performance against them is publicly reported, not to mention financial penalties levied on those whose numbers don’t measure up. In other words, doctor, we don’t trust you.
But just because you are confident doesn’t mean you’re correct. Just as being correct isn’t of great value if you don’t act on it with confidence. The answer would seem to be that physicians and staff being Confident AND Correct is the best way to ensure performance. In an industry that is utterly dependent on knowledge, being Confident and Correct when making care decisions is the best alternative to an oppressive Draconian system of regulatory oversight and fear-based motivation.
Prolific advances over the last 25 years in the brain science of how people learn and remember now make it possible to embed knowledge in people and commit it to long-term memory, at scale, without relying on extraordinary teachers available 24/7 or an oversight process that scares people into learning and remembering. I am not suggesting that physicians are infallible or that they know more than they do. In fact, in our work using Amplifire in healthcare so far, most physicians are confident and incorrect about 25-35% of what they need to know, and that needs to be and can be corrected.
Correcting misinformation is ultimately what The Joint Commission’s job is. But the JAMA article’s suggestion that beefing up The Joint Commission’s presence in hospitals to keep staff motivated to do the right things right more often is neither scalable nor sustainable. Offering hospitals and physicians a scalable way to stay current and continuously fend off misinformation so that physicians are both confident and correct is the best pathway to improving healthcare performance.
In the 1991 film called Defending Your Life, Albert Brooks plays a recently deceased man who is in a celestial weigh station where people defend the quality of their lives on earth as a way to make the case that they are worthy of advancing to the next level of existence in the universe. Brooks’ defense attorney Rip Torn explains to Brooks that, “the point of this whole thing is to keep getting smarter, to keep growing, to use as much of your brain as possible. Fear is like a giant fog, it just sits on your brain and blocks everything—real feelings, true happiness, real joy, they can’t get through that fog. But if you lift it, buddy, you’re in for the right of your life.”
That seems confident and correct to me.
-
10 Tips for Engaging and Aligning Physicians
30%. $2.4 trillion. 12 minutes. 1.8 million.
What do those numbers have in common? The answer is physicians:
- 30% of resources spent on healthcare have no impact on patient care, according to the Dartmouth Atlas Study.
- $2.4 trillion, or 80% of the annual US healthcare spend, is allocated based on decisions made by physicians.
- 12 minutes is the average amount of time that a typical physician spends per patient.
- 1.8 million scientific academic articles are published annually, and only half are read by anyone other than the author and the journal editor.
Getting and keeping physicians’ attention is critical, and very challenging. Influencing their decisions is even harder. Regardless, aligning physicians to make decisions that reduce variation and achieve the “Triple Aim” of delivering high quality, cost-effective care that meets patients’ expectations is a challenge every hospital or health system is faced with.
Most health systems know the challenge of physician alignment, but struggle to meaningfully engage their physicians. Most have physician liaison programs, web portals, forums with the chief medical officer, medical staff newsletters, and meetings, which provide part of the solution. What is often missing, however, is a scalable and sustainable way to keep physicians engaged.
Technology has the potential to serve as the spine of physician alignment because of its mobility, flexibility, personalization, dynamic modality, and immediacy. Used in combination with a well thought out strategy and effective engagement methods, technology offers a cost-effective, highly-scalable way to enable effective engagement and alignment.
But before you ask a physician to look at a mobile phone, download an app, read an email, open a file, attend a meeting, or change anything they’re doing, realize that there is a secret handshake among them, a password or algorithm that holds the key to getting and keeping their attention and making them open-minded to doing something differently.
Call it empathy, but we’ve learned through trial-and-error that there are 10 questions that physicians ask themselves before deciding to invest their limited time and attention:
1. Is it brief? Driven by throughput targets and other time-based pressures, a physician’s or provider’s day is lived in 12 minute increments. Make sure what you’re asking them to do isn’t too time consuming.
2. Is it credible? Whoever is asking for their time and attention must be a credible, recognized expert on the topic being addressed.
3. Is it current? The massive scope and rapid turnover of information that drives physician decisions requires that you understand the shortening shelf-life of what is considered current.
4. Is it engaging? If it’s true that physicians don’t have time to read, engage their other senses and use tools and methods to get and keep their attention. And remember, there is no better indication that a physician is engaged than when he or she is typing or talking. Ask yourself what will inspire him or her to do either.
5. Is it practical? If something asking for physicians’ time and attention is not action-able, and therefore not practical or relevant, it will be dismissed. Physicians don’t have time for theory.
6. Is it convenient? Don’t make them come to you. Make it easy for them to engage within their hectic and demanding day.
7. Is there too much? There are nearly 6,000 medical “apps”, 40,000 medical journals, 1 million medical blogs, and 12 million medical websites all vying for physicians’ attention. Hence, less is more.
8. Is it important? When everything is important, nothing is important. Physicians are desensitized to urgency, so understand what they consider to be urgent and why.
9. Is it transparent? Physicians are adept at percieving hidden agendas. Tell them what you want and why.
10. Is it safe? When they invest their time and attention, they want to know that their interests are protected—their reputation, personal information, and financial security.
Integrating these tactics into your engagement strategy will help align physicians in achieving the “Triple Aim” of healthcare.
