Boulder, CO — April 10, 2017 — We are pleased and proud to share the original Partners Healthcare blog post made by Amplifire advisor Robert Birnbaum, MD, PhD, who serves as Partners’ Vice President for Continuing Professional Development & Implementation Science.
Link to Partners blog: Partners Embraces Knowledge Engineering as Lynchpin of Healthcare Transformation posted by Robert Birnbaum M.D., Ph.D.
Healthcare transformation has upped the ante in regards to the maintenance of healthcare provider competency. New models of delivery, rapid information technology advances, and the ever-expanding velocity and veracity of clinical and research data, have led to an imperative need to adopt innovative approaches to life-long training of the healthcare provider workforce.
Unfortunately, many of the traditional methods of ensuring continual healthcare provider competency are antiquated, expensive or too labor intensive to be deployed with any regularity.
As healthcare systems shift to a value-based model, there’s a related need to quantify the impact of learning interventions and to foster more collaborative approaches to population management. “Knowledge engineering” refers to all the technical, scientific and social aspects involved in building, maintaining and using knowledge-based systems.
The Partners Office of Continuing Professional Development (Partners CPD) is unique among its peers for the emphasis it places on knowledge engineering as a guiding approach to address new healthcare competency assessment and remediation challenges. Partners CPD opened in 2012, and by 2015 it had disseminated approximately 4,000 hours of instruction to over 63,000 healthcare providers throughout Partners, all 50 states, and more than 38 countries. One example was a new “self-study” format that focused on a mandate from the Massachusetts Board of Registration, to enhance provider competency in “Pain Management & Opioid Prescribing” and “End of Life Care.” Ultimately, this approach helped over 6,800 Massachusetts physicians fulfill their relicensing requirements.
Partners CPD Healthcare Knowledge Transformation Laboratory expands upon this foundation by serving as an R&D accelerator to architect, build, and test cutting-edge learning innovations. The lab works closely with Partners internal capabilities, coupling them with technology startups, innovation collaborators, and service healthcare stakeholders, to deliver specific goals (e.g., improving diagnostic accuracy, reducing avoidable harm, leveling disparities in care, etc.) (See figure 1).
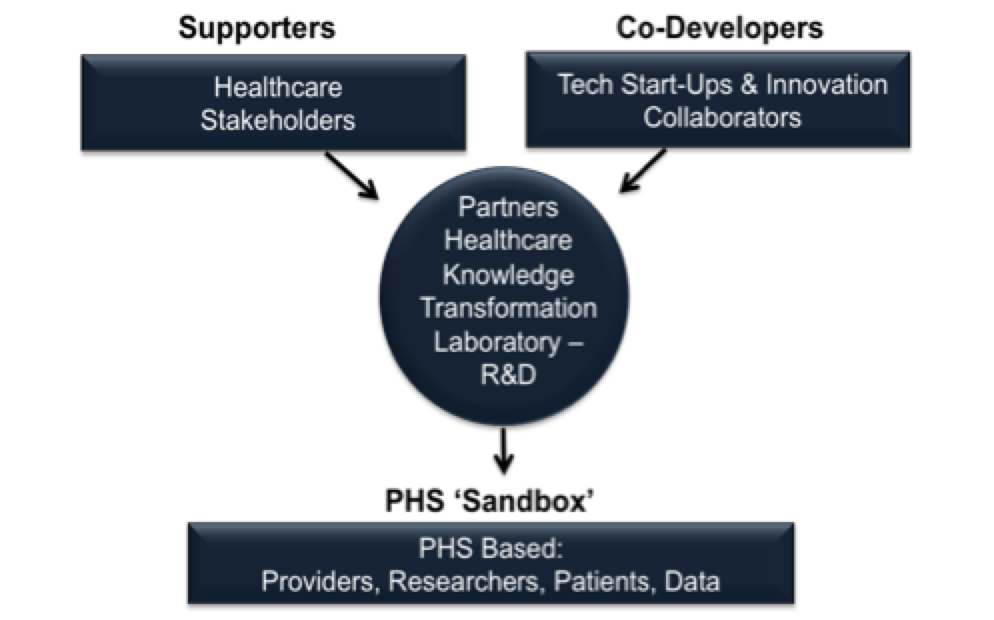
Figure 1: Partners Knowledge Transformation Laboratory.
A central principle of these innovations is to connect learning with tangible process improvement. It’s no secret that our industry has a long history of wasteful investments that nurture training approaches without a demonstrable improvement to quality care. Therefore, it’s important to both foster the application of evidence-based protocols and to execute the iterative learning interventions that will assure the adoption of those protocols close to the point of care. Learning interventions that have traditionally taken healthcare providers “off line” to regional conventions, or have had them passively spend hours watching webinars, only add to their administrative burden and have a tenuous link to their day-to-day clinical practices.
Today, technological advances enable instructional designers to embed learning interventions within workflows, which ultimately lead to the creation of micro-learning environments. More constricted resource allocations warrant balancing when to target sub-optimally performing individuals for remediation versus leveraging machine-assisted human intelligence (e.g. clinical decision support), and how to economize individual interventions by customizing them—which stands in contrast to bombarding everyone with the same information. Learning interventions must incorporate basic principles of cognitive psychology and neuroscience (i.e. how the brain learns) in order to assure the retention and utilization of information.

Figure 2: The elements of learning interventions driving healthcare process improvement.
Lastly, enterprise clinical data repositories, derived from electronic health record (EHR) systems, accrue vast amounts of vital disease management data that can be made relational to learning interventions, in order to measure their impact.
Partners CPD strives to create a virtuous learning process/improvement cycle, comprised of low friction proficiency assessments of healthcare providers, customized learning interventions, and validated impact metrics (See figure 2).
Moving forward, we’re confident that these advances in knowledge engineering will create a dynamic learning healthcare system that is responsive to the emerging needs of both healthcare providers and patients alike.
Robert J. Birnbaum, M.D., Ph.D. is the Vice President for Continuing Professional Development & Implementation Science at Partners Healthcare and Assistant Professor of Psychiatry at Harvard Medical School. Dr. Birnbaum is a practicing and supervising psychopharmacologist affiliated with the Psychiatry Department at Massachusetts General Hospital.
His Ph.D. research was in physiology/biochemistry studying intracellular signal transduction and his post-doctoral research was in molecular neurogenetics studying psychotropic drug induction of neural immediate early gene expression. Dr. Birnbaum serves as primary liaison for Partners Healthcare to the American Board of Medical Specialties (ABMS) for the Multispecialty Portfolio Program and collaborates with the ABMS Education & Research Foundation. Dr. Birnbaum served on the standing committee for continuing medical education at Harvard Medical School, the Foundation Board of the Alliance for Continuing Education in the Health Professions, and the Education Research Committee of the Society for Academic Continuing Medical Education. Dr. Birnbaum also serves on the Partners Educational Review Board and is on the faculty of the Harvard Macy Institute, leading workshops on healthcare education innovation. He has collaborated on education research projects with the MIT Integrative Learning Initiative (MITili), the Shanghai Mental Health Center (SHMHC), the Institute of Mental Health (IMH) at Peking University (PKU), and the Sydney West Australia Translational Cancer Research Center. He is Co-Chair of the Lunder Dineen Health Education Alliance of Maine.
Dr. Birnbaum’s current research focuses on knowledge translation and implementation science in the health professions, particularly the application of cognitive psychology and basic neuroscience principles to instructional design and knowledge engineering.